Urinary tract infection
Highlights
Urinary Tract Infections (UTIs)
Urinary tract infections (UTIs) are a common type of infection caused by bacteria (most often E. coli) that travel up the urethra to the bladder. A bladder infection is called cystitis. If bacterial infection spreads to the kidneys and ureters, the condition is called pyelonephritis. Cystitis is considered a lower urinary tract infection. Pyelonephritis is an upper urinary tract infection and is much more serious.
Risk Factors
Women are more susceptible to urinary tract infections than men, and their infections tend to recur. One reason is that the urethra (the tube that carries urine away from the bladder) is shorter in women than in men. Frequent sexual intercourse also increases a woman’s risk of developing UTIs. Contraceptive spermicides and diaphragm use are other risk factors. When women reach menopause, the decrease in estrogen thins the lining of the urinary tract, which increases susceptibility to bacterial infections.
Pregnancy does not increase the risk of getting a urinary tract infection but it can increase the risk of developing a serious infection that could potentially harm the mother and fetus. Pregnant women should report any symptoms of UTIs to their doctors, and should get screened for asymptomatic bacteriuria (presence of significant numbers of bacteria without symptoms).
Symptoms
Symptoms of urinary tract infections may include:
- Strong urge to urinate frequently, even immediately after the bladder is emptied
- Painful burning sensation when urinating
- Discomfort, pressure, or bloating in the lower abdomen
- Pain in the pelvic area or back
- Cloudy or bloody urine, which may have a strong smell
A urine test can determine if these symptoms are caused by a bacterial infection. Antibiotics are used to treat UTIs. Older people may have a urinary tract infection but have few or no symptoms.
Treatment
Antibiotics are used to treat UTIs. Most cases of UTIs clear up after a few days of drug treatment, but more severe cases may require several weeks of treatment.
Guidelines recommend using nitrofurantoin or trimethoprin-sulfamethoxazole as first-line antibiotic treatments for UTIs. Fluoroquinolones (such as ciprofloxacin) are now only recommended when other antibiotics are not appropriate.
Cranberries for UTI Protection
Cranberry products may help prevent UTIs in some women especially those with recurrent infections, indicates a 2012 review of studies. Drinking several glasses of cranberry juice a day appeared to offer more protection than taking cranberry tablets. Researchers think that cranberries help prevent harmful bacteria from attaching and sticking to urinary tract cells.
Introduction
A urinary tract infection (UTI) is a condition in which one or more parts of the urinary system (the kidneys, ureters, bladder, and urethra) become infected. UTIs are the most common of all bacterial infections and can occur at any time in the life of an individual. Nearly 95% of cases of UTIs are caused by bacteria that typically multiply at the opening of the urethra and travel up to the bladder. Much less often, bacteria spread to the kidney from the bloodstream.
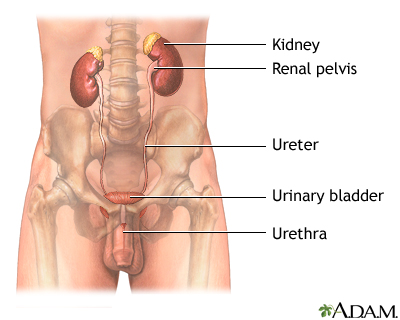
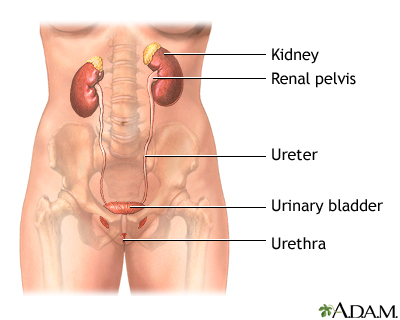
The Urinary System. The urinary system helps maintain proper water and salt balance throughout the body and also expels urine from the body. It is made up of the following organs and structures:
- The two kidneys, located on each side below the ribs and toward the middle of the back, play the major role in this process. They filter waste products, water, and salts from the blood to form urine.
- Urine passes from each kidney to the bladder through thin tubes called ureters.
- Ureters empty the urine into the bladder, which rests on top of the pelvic floor. The pelvic floor is a muscular structure similar to a sling running between the pubic bone in front to the base of the spine.
- The bladder stores the urine. When the bladder becomes filled, the muscle in the wall of the bladder contracts, and the urine leaves the body via another tube called the urethra. In men the urethra is enclosed in the penis. In women, it leads directly out.
Defense Systems Against Bacteria. Infection does not always occur when bacteria are introduced into the bladder. A number of defense systems protect the urinary tract against infection-causing bacteria:
- Urine functions as an antiseptic, washing potentially harmful bacteria out of the body during normal urination. (Urine is normally sterile, that is, free of bacteria, viruses, and fungi.)
- The ureters join into the bladder in a manner designed to prevent urine from backing up into the kidney when the bladder squeezes urine out through the urethra.
- The prostate gland in men secretes infection-fighting substances.
- The immune system defenses and antibacterial substances in the mucous lining of the bladder eliminate many organisms.
- In healthy women, the vagina is colonized by lactobacilli, beneficial microorganisms that maintain a highly acidic environment (low pH) that is hostile to other bacteria. Lactobacilli produce hydrogen peroxide, which helps eliminate bacteria and reduces the ability of Escherichia coli (E. coli) to adhere to vaginal cells. (E. coli is the major bacterial culprit in urinary tract infections.)
Types of UTIs. UTIs are generally classified as:
- Uncomplicated or complicated, depending on the factors that trigger the infections
- Primary or recurrent, depending on whether the infection is occurring for the first time or is a repeat event
Uncomplicated Urinary Tract Infections (UTIs)
Uncomplicated UTIs are due to a bacterial infection, most often E. coli. They affect women much more often than men.
Cystitis. Cystitis, or bladder infection, is the most common urinary tract infection. It occurs in the lower urinary tract (the bladder and urethra) and nearly always in women. In most cases, the infection is brief and acute and only the surface of the bladder is infected. Deeper layers of the bladder may be harmed if the infection becomes persistent, or chronic, or if the urinary tract is structurally abnormal.
Pyelonephritis (Kidney Infection). Sometimes the infection spreads to the upper tract (the ureters and kidneys). This is called pyelonephritis, or more commonly, a kidney infection.
Complicated Urinary Tract Infections
Complicated infections, which occur in men and women of any age, are also caused by bacteria but they tend to be more severe, more difficult to treat, and recurrent. They are often the result of:
- Some anatomical or structural abnormality that impairs the ability of the urinary tract to clear out urine and therefore bacteria.
- Catheter use in the hospital setting or chronic indwelling catheter in the outpatient setting,
- Bladder and kidney dysfunction, or kidney transplant (especially in the first 3 months after transplant).
Recurrences can occur in patients with complicated UTI if the underlying structural or anatomical abnormalities are not corrected.
Recurrent Urinary Tract Infections
Most women who have had an uncomplicated UTI have occasional recurrences. About 25 - 50% of these women can expect another infection within a year of the previous one. Between 3 - 5% of women have ongoing, recurrent urinary tract infections, which follow the resolution of a previous treated or untreated episode.
Recurrence is often categorized as either reinfection or relapse:
- Reinfection. Most cases of recurring UTIs are reinfections. A reinfection occurs several weeks after antibiotic treatment has cleared up the initial episode and can be caused by the same bacterial strain that caused the original episode or a different one. The infecting organism is usually introduced through fecal bacteria and moves up through the urinary tract.
- Relapse. Relapse is the less common form of recurrent urinary tract infection. It is diagnosed when a UTI recurs within 2 weeks of treatment of the first episode and is due to treatment failure. Relapse usually occurs in kidney infection (pyelonephritis) or is associated with obstructions such as kidney stones, structural abnormalities or, in men, chronic prostatitis.
Asymptomatic Urinary Tract Infection (Asymptomatic Bacteriuria)
When a person has no symptoms of infection but significant numbers of bacteria have colonized the urinary tract, the condition is called asymptomatic UTI (also called asymptomatic bacteriuria). The condition is harmless in most people and rarely persists, although it does increase the risk for developing symptomatic UTIs.
Screening for asymptomatic bacteriuria is not necessary during most routine medical examinations, with the following exceptions:
- Pregnant women. Pregnant women with asymptomatic bacteriuria have an increased risk of acute pyelonephritis in their second or third trimester. Therefore, they need screening and treatment for this condition. Guidelines recommend that pregnant women be screened for asymptomatic bacteriuria at 12 - 16 weeks gestation or at the first pre-natal visit, if later.
- People undergoing urologic surgery (such as prostate surgery in men). The presence of an infection during surgery can lead to serious consequences.
Causes
The bacterial strains that cause UTIs include:
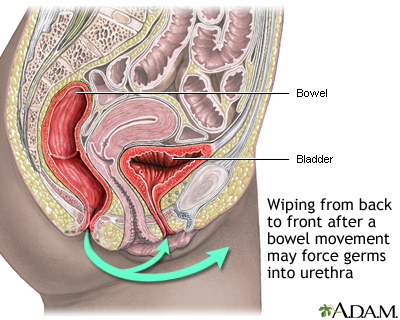
- Escherichia (E.) coli is responsible for most uncomplicated cystitis cases in women, especially in younger women. E. coli is generally a harmless microorganism originating in the intestines. If it spreads to the vaginal opening, it may invade and colonize the bladder, causing an infection. The spread of E. coli to the vaginal opening most commonly occurs when women or girls wipe themselves from back to front after urinating, or after sexual activity.
- Staphylococcus saprophyticus accounts for 5 - 15% of UTIs, mostly in younger women.
- Klebsiella, Enterococci, and Proteus mirabilis account for most of remaining bacterial organisms that cause UTIs. They are generally found in UTIs in older women.
- Rare bacterial causes of UTIs include Ureaplasma urealyticum and Mycoplasma hominis, which are typically harmless organisms.
Organisms in Severe or Complicated Infections
- The bacteria that cause kidney infections (pyelonephritis) are generally the same bacteria that cause cystitis. There is some evidence, however, the E. coli strains in pyelonephritis are more virulent (able to spread and cause illness).
- Complicated UTIs that are related to physical or structural conditions are apt to be caused by a wider range of organism. E. coli is still the most common organism, but others include Klebsiella, P. mirabilis, and Citrobacter.
- Fungal organisms, such as Candida species. (Candida albicans causes the "yeast infections" that also occur in the mouth, digestive tract, and vagina.)
- Other bacteria associated with complicated or severe infection include Pseudomonas aeruginosa, Enterobacter, and Serratia species gram-positive organisms (including Enterococcus species).
Bacterial Strains in Recurrent UTIs
Recurring infections are often caused by different bacteria than those that caused a previous or first infection.
Factors in Overcoming the Bacterial Defense Systems
Changes in the amount or type of acid within the genital and urinary tracts contribute to lowering the resistance to infection. For example, beneficial organisms called lactobacilli increase the acidic environment in the female urinary tract. Reductions in their number (which, for example, occur with estrogen loss after menopause), increase pH and therefore the risk of infection.
Risk Factors
After the flu and common cold, urinary tract infections (UTIs) are the most common medical complaint among women in their reproductive years. UTIs are far more common among women than among men. Most women will develop a UTI at some time in their lives, and many will have recurrences.
Specific Risk Factors in Women
Structure of the Female Urinary Tract. In general, the higher risk in women is mostly due to the shortness of the female urethra, which is 1.5 inches compared to 8 inches in men. Bacteria from fecal matter at the anal opening can be easily transferred to the opening of the urethra.
Sexual Behavior. Frequent or recent sexual activity is the most important risk factor for urinary tract infection in young women. Nearly 80% of all urinary tract infections in premenopausal women occur within 24 hours of intercourse. UTIs are very rare in celibate women. However, UTIs are NOT sexually transmitted infections.
In general, it is the physical act of intercourse itself that produces conditions that increase susceptibility to the UTI bacteria, with some factors increasing the risk. For example, women having sex for the first time or who have intense or frequent sex are at risk for a condition called "honeymoon cystitis."
Certain types of contraceptives can also increase the risk of UTIs. In particular, women who use diaphragms tend to develop UTIs. The spring-rim of the diaphragm can bruise the area near the bladder, making it susceptible to bacteria. Spermicidal foam or gel used with diaphragms, and spermicidal-coated condoms, also increase susceptibility to UTIs. Most spermicides contain nonoxynol-9, a chemical that is associated with increased UTI risk.
Pregnancy. In pregnant women, the presence of asymptomatic bacteriuria is associated with increased risk of kidney infection, which can cause early labor and other serious pregnancy complications. For this reason, pregnant women should be screened and treated for asymptomatic bacteriuria. Pregnant women are more susceptible to kidney infection because as the uterus enlarges it compresses the ureters and bladder. This causes urine to back up into the kidney, increasing the risk of bacterial infection.
Menopause. The risk for UTIs, both symptomatic and asymptomatic, is highest in women after menopause. This is primarily due to decrease in estrogen, which thins the walls of the urinary tract and reduces its ability to resist bacteria. Estrogen loss can also reduce certain immune factors in the vagina that help block E. coli from adhering to vaginal cells. For some women, topical estrogen therapy helps restore healthy bacteria and reduce the risk of recurrent UTIs. (Oral hormone replacement therapy is not helpful for UTIs.)
Other aging-related urinary conditions, such as urinary incontinence, can increase the risk for recurrent urinary tract infections.
Allergies. Women who have skin allergies to ingredients in soaps, vaginal creams, bubble baths, or other chemicals that are used in the genital area are at increased risk for UTIs. In such cases, the allergies may cause small injuries that can introduce bacteria.
Antibiotic Use. Antibiotics often eliminate lactobacilli, the protective bacteria, along with harmful bacteria. This can cause an overgrowth of E. coli in the vagina.
Specific Risk Factors in Men
Men become more susceptible to UTIs after age 50, when they begin to develop prostate problems. Benign prostatic hyperplasia (BPH), enlargement of the prostate gland, can produce obstruction in the urinary tract and increase the risk for infection. In men, recurrent urinary tract infections are also associated with prostatitis, an infection of the prostate gland. Although only about 20% of UTIs occur in men, these infections can cause more serious problems than they do in women. Men with UTIs are far more likely to require hospitalization than women.
Specific Risk Factors in Children
Each year, about 3% of American children develop urinary tract infections. During the first few months of life, UTIs are more common in boys than in girls. Boys who are uncircumcised are about 10 - 12 times more likely than circumcised boys to develop UTIs by the time they are 1 year old. After the age of 2 years, UTIs are far more common in girls. As with adults, E. coli is the most common cause of UTIs in children.
Vesicoureteral Reflux (VUR). Vesicoureteral reflux (VUR) is the cause of up to half of urinary tract infections that occur during childhood. VUR also puts children at risk for UTI recurrence.
VUR is a condition in which the urine backs up into the kidneys. Normally, when the bladder becomes filled, the muscle in the wall of the bladder contracts, and the urine leaves the body via another tube called the urethra. There is a valve-like mechanism where the ureters join the bladder. These valves' job is to keep urine from flowing backward towards the kidneys when the bladder contracts. If the valves do not work well, urine may remain in the bladder where bacteria can grow. The back flow of urine may also carry any infection from the bladder up into the kidneys.
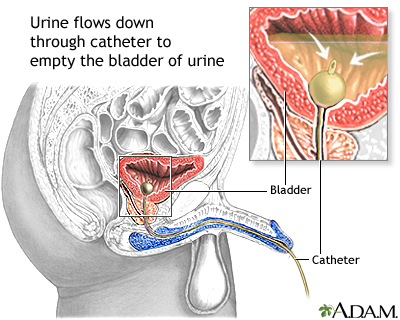
Catheterization and UTI Risk
Most UTIs that develop in hospitalized patients are due to urinary catheters. The longer any urinary catheter is in place, the higher the risk for growth of bacteria and an infection. In most cases of catheter-induced UTIs, there are no symptoms. Because of the risk for wider infection, however, anyone requiring a catheter should be screened for infection. Catheters should be used only when necessary and should be removed as soon as possible.
All older adults who are immobilized, catheterized, or dehydrated are at increased risk for UTIs. Nursing home residents, particularly those who are incontinent, are at very high risk.
Medical Conditions that Increase the Risk of UTIs
Diabetes. Diabetes puts women at significantly higher risk for asymptomatic bacteriuria. The longer a woman has diabetes, the higher the risk. (Control of blood sugar does not affect this condition.) The risk for UTI complications, and fungal-related UTIs, is also higher in people with diabetes.
Kidney Problems. Nearly any kidney disorder, including kidney stones, increases the risk for complicated UTIs.
Neurogenic Bladder. A number of brain and nerve disorders can affect the nerves of the bladder and cause problems with the ability to empty the bladder and control urine leakage. Multiple sclerosis, stroke, spinal cord injury, and diabetic neuropathy are common examples.
Sickle-Cell Anemia. Patients with sickle-cell anemia are particularly susceptible to kidney damage from their disease, and UTIs put them at even greater risk.
Immune System Problems. People with immunocompromised systems, such as those who have HIV/AIDS or who are undergoing treatment for cancer, are at increased risk for all types of infections, including UTIs and pyelonephritis.
Urinary Tract Abnormalities. Some people have structural abnormalities of the urinary tract that cause urine to stagnate or flow backward into the upper urinary tract. A prolapsed bladder (cystocele) can result in incomplete urination so that urine collects, creating a breeding ground for bacteria. Tiny pockets called diverticula sometimes develop inside the urethral wall and can collect urine and debris, further increasing the risk for infection.
Complications
In most cases, urinary tract infections are annoyances that cause urinary discomfort. However, if left untreated, UTIs can develop into very serious and potentially life-threatening kidney infections (pyelonephritis) that can permanently scar or damage the kidneys. The infection may also spread into the bloodstream (called sepsis) and elsewhere in the body.
UTIs in pregnant women pose serious health risks for both mother and child. UTIs that occur during pregnancy pose a higher than average risk of developing into kidney infections. Any pregnant woman who suspects she has a urinary tract infection should immediately contact her doctor. Many doctors recommend that women receive periodic urine testing throughout their pregnancies to check for signs of bacterial infection.
In some adults, recurrent UTIs may cause scarring in the kidneys, which over time can lead to renal hypertension and eventual kidney failure. Most of these adults with kidney damage have other predisposing diseases or structural abnormalities. Recurrent urinary tract infections, even in the kidney, almost never lead to progressive kidney damage in otherwise healthy women.
Scarring and future kidney problems are also concerns for children who experience severe or multiple kidney infections.
Symptoms
Symptoms of lower urinary tract infections usually begin suddenly and may include one or more of the following signs:
- The urge to urinate frequently, which may recur immediately after the bladder is emptied.
- A painful burning sensation when urinating. (If this is the only symptom, then the infection is most likely urethritis, an infection limited to the urethra.)
- Discomfort or pressure in the lower abdomen. The abdomen can feel bloated.
- Pain in the pelvic area or back.
- The urine often has a strong smell, looks cloudy, or contains blood. This is a sign of pyuria, or a high white blood cell count in the urine, and is a very reliable indicator of urinary tract infections.
- Occasionally, fever develops.
Symptoms of Severe Infection in the Kidney (Pyelonephritis)
Symptoms of kidney infections tend to affect the whole body and be more severe than those of cystitis (inflammation of the bladder and ureters). They may include:
- Symptoms of lower UTIs that persist longer than a week. (Sometimes lower UTI symptoms may be the only signs of kidney infection. People at highest risk for such "silent" upper urinary tract infections include patients with diabetes, impaired immune systems, or a history of relapsing or recurring UTIs.)
- An increased need to urinate at night.
- Chills and persistent fever (typically lasting more than 2 days).
- Pain in the flank (pain that runs along the back at about waist level).
- Vomiting and nausea.
Symptoms of UTIs in Infants and Toddlers
UTIs in infants and preschool children tend to be more serious because they are more likely to involve the kidneys. (Older children are more likely to have lower urinary tract infections and standard symptoms.) Infants and young children should always be checked for UTIs if the following symptoms are present:
- A persistent high fever of otherwise unknown cause, particularly if it is accompanied by signs of feeding problems, listlessness and fatigue.
- Painful, frequent, and foul smelling urine. (Parents are generally unable to identify a UTI just by the smell of their child's urine. Medical tests are needed.)
- Cloudy urine. (If the urine is clear, the child most likely has some other ailment, although it is not absolute proof that the child is UTI-free.)
- A recurrence of bedwetting or poor urine control during the day in the child who had previously achieved control.
- Abdominal and low back pain may be present.
- Vomiting and abdominal pain (usually in infants).
Symptoms of UTIs in Older Patients
The classic lower UTI symptoms of pain, frequency, or urgency and upper tract symptoms of flank pain, chills, and tenderness may be absent or altered in older patients with UTIs.
Symptoms of UTIs that may occur in seniors but not in younger adults may include mental changes or confusion, nausea or vomiting, abdominal pain, or cough and shortness of breath. Concomitant illness may further confuse the picture and make diagnosis difficult.
Diagnosis
A doctor can confirm if you have a urinary tract infection by testing a sample of your urine. For some younger women who are at low risk of complications, the doctor may not order a urine test and may diagnose a urinary tract infection based on the description of symptoms.
Urine Tests
Urinalysis. A urinalysis is an evaluation of various components of a urine sample. It involves looking at the urine color and clarity, using a special dipstick to do different chemical testing, and possibly inspecting some of the urine underneath a microscope. A urinalysis usually provides enough information for a doctor or nurse to start treatment.
Urine Culture. If necessary, the doctor may order a urine culture, which involves incubating and growing the bacteria contained in the urine. A urine culture can help identify the specific bacteria causing the infection, and determine which type of antibiotics to use for treatment. A urine culture may be ordered if the urinalysis does not show signs of infection but the doctor still suspects a UTI is causing the symptoms. It may also be ordered if the doctor suspects complications from the infection.
Clean-Catch Sample. To obtain an untainted urine sample, doctors usually request a so-called midstream, or clean-catch, urine sample. To provide this, the following steps are taken:
- Wash your hands thoroughly, then wash the penis or vulva and surrounding area four times, with front-to-back strokes, using a new soapy sponge each time.
- Urinate a small amount into the toilet for a few seconds and then stop. (Women should hold open with one hand the folds of the labia while urinating.)
- Position the container to catch the middle portion of the stream. Urinate until the collection cup is halfway full (about 2 ounces).
- Remove the cup and urinate the remainder of your flow into the toilet.
- Securely screw the container cap in place without touching the inside of the rim and place it where directed. The sample will be given to the doctor or sent to the laboratory for analysis.
Collection with a Catheter. Some patients (small children, elderly people, or hospitalized patients) cannot provide a urine sample. In such cases, a catheter may be inserted into the bladder to collect urine. This is the best method for providing a contaminant-free sample, but it carries a risk of introducing or spreading infection.
Other Tests
If the infection does not respond to treatment, the doctor may order other tests to determine what is causing symptoms. Imaging tests such as ultrasound and computed tomography can help identify:
- Serious and recurrent cases of pyelonephritis
- Structural abnormalities
- Obstruction (such as kidney stones) or abscess
- Possible obstruction or vesicoureteral reflux in children ages 2 - 24 months
Special Types of X-Rays. Special x-rays can be used to screen for structural abnormalities, urethral narrowing, or incomplete emptying of the bladder:
- Voiding cystourethrogram is an x-ray of the bladder and urethra. To obtain a cystourethrogram, a dye, called contrast material, is injected through a catheter inserted into the urethra and passed through the bladder.
- An intravenous pyelogram (IVP) is an x-ray of the kidney. For a pyelogram, the contrast matter is injected into a vein and eliminated by the kidneys. In both cases, the dye passes through the urinary tract and reveals any obstructions or abnormalities on x-ray images.
Cystoscopy. Cystoscopy is used to detect structural abnormalities, interstitial cystitis, or masses that might not show up on x-rays during an IVP. The patient is given a light anesthetic, and the bladder is filled with water. The procedure uses a cystoscope, a flexible, tube-like instrument that the urologist inserts through the urethra into the bladder.
Blood Cultures. If the patient has fever or other signs of a serious infection, the doctor will order blood cultures to determine if the infection has entered the bloodstream and is threatening other parts of the body.
Ruling Out Conditions with Similar Symptoms
About half of women with symptoms of a UTI actually have some other condition, such as irritation of the urethra, vaginitis, interstitial cystitis, or sexually transmitted diseases (STDs). Some of these problems may also accompany or lead to UTIs.
Vaginitis. Vaginitis is a common vaginal infection that can be caused by a yeast (candidiasis) or bacteria. Occasionally, the infection causes frequent urination, mimicking cystitis. The typical symptoms of vaginitis are itching and an abnormal discharge.
Sexually Transmitted Diseases. Women with painful urination whose urine does not exhibit signs of bacterial growth in culture may have a sexually transmitted disease. The most common microorganism is Chlamydia trachomatis. Other STDs that may be responsible include gonorrhea and genital herpes.
Interstitial Cystitis. Interstitial cystitis (IC) is an inflammation of the bladder wall that occurs almost predominantly in women. The average age of patients with IC is 40 years old, but 25% of cases occur in women under age 30. Symptoms are very similar to cystitis, but no bacteria are present. Pain during sex is a very common complaint in these patients, and stress may intensify symptoms.
Kidney Stones. The pain of kidney stones along with blood in the urine can resemble the symptoms of pyelonephritis. There are no bacteria present with kidney stones, however.
Thinning Urethral and Vaginal Walls. After menopause, the vaginal and urethral walls become dry and fragile, causing pain and irritation that can mimic a UTI.
Disorders in Children that Mimic UTIs. Problems that might cause painful urination in children include reactions to chemicals in bubble bath, diaper rashes, and infection from the pinworm parasite.
Prostate Conditions in Men. Prostate conditions, including prostatitis (inflammation of the prostate) and benign prostatic hyperplasia, can cause symptoms similar to urinary tract infections.
Treatment
Antibiotics are the main treatment for all UTIs. A variety of antibiotics are available, and choices depend on many factors, including whether the infection is complicated or uncomplicated or primary or recurrent. Treatment decisions are also based on the type of patient (man or woman, a pregnant or nonpregnant woman, child, hospitalized or nonhospitalized patient, or person with diabetes). A doctor may also select an antibiotic based on the resistance rate in that geographic area. Treatment should not necessarily be based on the actual bacteria count. For example, if a woman has symptoms, even if bacterial count is low or normal, infection is probably present, and the doctor should consider antibiotic treatment.
Treatment for Uncomplicated UTIs
UTIs can often be successfully treated with antibiotics prescribed over the phone. In such cases, a health professional provides the patients with 3-day antibiotic regimens without requiring an office urine test. This course is recommended only for women who have typical symptoms of cystitis, who are at low risk for recurrent infection, and who do not have symptoms (such as vaginitis) suggesting other problems.
Antibiotic Regimen. Oral antibiotic treatment cures nearly all uncomplicated urinary tract infections, although the rate of recurrence remains high. The following antibiotics are commonly used for uncomplicated UTIs:
- The standard regimen is a 3-day course of trimethoprim-sulfamethoxazole, commonly called TMP-SMX (Bactrim, Septra, generic). TMP-SMX combines an antibiotic with a sulfa drug. A single dose of TMP-SMX is sometimes prescribed in mild cases, but cure rates are generally lower than with 3-day regimens. Allergies to sulfa are common and may be serious.
- Nitrofurantoin (Furadantin, Macrobid, Macrodantin, generic) is another first-line option. It is usually taken daily for 5 days.
- Fosfomycin (Monurol) is not as effective as other antibiotics but may be used during pregnancy. Resistance rates to this drug are very low.
- Fluoroquinolone antibiotics, also called quinolones, are only recommended for UTIs when other antibiotics cannot be used. Ciprofloxacin (Cipro, generic) is the quinolone antibiotic most commonly prescribed. Quinolones are usually given over a 3-day period. Pregnant women should not take these drugs.
- Other antibiotics may also be used, including amoxicillin-clavulanate cefdinir, cefaclor, and cefpodoxime-proxetil. These drugs may be prescribed when other antibiotics are not appropriate. They are usually given in 3 - 7 day regimens.
After a week of antibiotic treatment, most patients are free of infection. If the symptoms do not clear up within the first few days of therapy, doctors generally suggest that women discontinue their antibiotic and provide a urine sample for culturing in order to identify the specific organism causing the condition.
Treatment for Relapsing Infection. A relapsing infection (caused by treatment failure) occurs within 3 weeks in about 10% of women. Relapse is treated similarly to a first infection, but the antibiotics are usually continued for 7 - 14 days. (Relapsing infections may be due to structural abnormalities, abscesses, or other problems that may require surgery, and such conditions should be ruled out.)
Treatment for Recurrent Infections
Women who have two or more symptomatic UTIs within 6 months or three or more over the course of a year may need preventive antibiotics. A woman's own perception of discomfort can generally guide her decisions on whether or not to use preventive antibiotics. All women should use lifestyle measures to prevent recurrences.
Intermittent Self Treatment. Many, if not most, women with recurrent UTIs can effectively self-treat recurrent UTIs without going to a doctor. In general, this requires the following steps:
- As soon as the patient develops symptoms, she takes the antibiotic. Infections that occur less than twice a year are usually treated as if they were an initial attack, with single-dose or 3-day antibiotic regimens.
- In some cases, she also performs a clean-catch urine test before starting antibiotics and sends it to the doctor for culturing to confirm the infection.
A woman should consult a doctor under the following circumstances:
- If symptoms have not gone away within 48 hours
- If there is a change in symptoms
- If the patient suspects that she is pregnant
- If the patient has more than four infections a year
Women who are not good candidates for self-treatment are those with impaired immune systems, previous kidney infections, structural abnormalities of the urinary tract, or a history of infection with antibiotic-resistant bacteria.
Postcoital Antibiotics. If recurrent infections are clearly related to sexual activity and episodes recur more than two times within a 6-month period, a single preventive dose taken immediately after intercourse is effective. Antibiotics for such cases include TMP-SMX, nitrofurantoin, cephalexin, or a fluoroquinolone (such as ciprofloxacin). (Fluoroquinolones are not appropriate during pregnancy.)
Continuous Preventive Antibiotics (Prophylaxis). Continuous preventive (prophylactic) antibiotics are an option for some women who do not respond to other measures. With this approach, low-dose antibiotics are taken continuously for 6 months or longer.
Treatment for Kidney Infections (Pyelonephritis)
Patients with uncomplicated kidney infections (pyelonephritis) may be treated at home with oral antibiotics. Ciprofloxacin (Cipro, generic) or another fluoroquinolone is typically given but other antibiotics, such as trimethoprim-sulfamethoxazole, may be used. Patients with moderate-to-severe acute kidney infection and those with severe symptoms or other complications may need to be hospitalized. In such cases, antibiotics are usually given intravenously for several days. Chronic pyelonephritis may require long-term antibiotic treatment.
Treatments for Specific Populations
Treating Pregnant Women. Pregnant women should be screened for UTIs, since they are at high risk for UTIs and their complications. The antibiotics used during pregnancy include amoxicillin, ampicillin, nitrofurantoin, and cephalosporins. Fosfomycin (Monurol) is not as effective as others but may be used during pregnancy. In general, there is no consensus on which antibiotic is best for pregnant women although some types of antibiotics, such as fluoroquinolones and tetracyclines, should not be taken as they can cause harm to the fetus.
Pregnant women with asymptomatic bacteriuria (evidence of infection but no symptoms) have a 30% risk for acute pyelonephritis in their second or third trimester. They need screening and treatment for this condition. In such cases, they should be treated with a short course of antibiotics (3 - 5 days). For an uncomplicated UTI, pregnant women may need longer-term antibiotics (7 - 10 days).
Treating Children with UTIs. Children with UTIs are generally treated with TMP-SMX, cephalexin (Keflex, generic) and other cephalosporins, or amoxicillin/clavulanic acid (Augmentin, generic). These drugs are usually taken by mouth in either liquid or pill form. Doctors sometimes give them as a shot or IV. Children usually respond to treatment within a few days.
Vesicoureteral reflux (VUR) is a concern for children with UTIs. (See Risk Factors section.) VUR can lead to kidney infection (pyelonephritis), which can cause kidney damage. The two treatment options for children with VUR are long-term antibiotics to prevent infections or surgery to correct the condition. However, there is debate as to the benefit of these approaches. Current guidelines advise that antibiotics do not really help prevent recurrent urinary tract infections in children, and that VUR itself may not substantially increase the risk for recurrent UTI
Children with acute kidney infection are treated with various antibiotics including oral cefixime (Suprax) or a short course (2 - 4 days) of an intravenous (IV) antibiotic (typically gentamicin, given in one daily dose). An oral antibiotic then follows the IV.
Management of Catheter-Induced Urinary Tract Infections
Catheter-induced urinary tract infections are very common, and preventive measures are extremely important. In-dwelling catheters should not be used unless absolutely necessary, and they should be removed as soon as possible. Reducing the risk for infections during long-term catheter use, however, remains problematic. For men, condom catheters may be an alternative to indwelling catheters.
Daily Hygiene. A typical catheter is one that has been preconnected and sealed and uses a drainage bag system. To prevent infection, some of the following tips may be helpful:
- Drink plenty of fluids.
- The catheter tube should be free of any knots or kinks.
- Clean the catheter and the area around the urethra with soap and water daily and after each bowel movement. (Women should be sure to clean front to back.)
- Wash hands before touching the catheter or surrounding area.
- Never disconnect the catheter from the drainage bag without careful instructions from a health professional on strict methods for preventing infection.
- Keep the drainage bag off the floor.
- Stabilize the bag against the leg using tape or some other system.
Antibiotics for Catheter-Induced Infections. Patients using catheters who develop UTIs with symptoms should be treated for each episode with antibiotics and the catheter should be removed, if possible, or changed. A major problem in treating catheter-related UTIs is that the organisms involved are constantly changing. Because there are likely to be multiple species of bacteria, doctors generally recommend an antibiotic that is effective against a wide variety of microorganisms.
Although high bacteria counts in the urine (bacteriuria) occur in most catheterized patients, administering antibiotics to prevent a UTI is rarely recommended. Many catheterized patients do not develop symptomatic urinary tract infections even with high bacteria counts. If bacteriuria occurs without symptoms, antibiotic therapy has little benefit if the catheter is to remain in place for a long period.
Medications
Although antibiotics are the first treatment choice for urinary tract infections, antibiotic-resistant strains of E. coli, the most common cause of UTIs, are increasing worldwide. As more bacteria have become resistant to the standard UTI treatment trimethoprim-sulfamethoxazole (TMP-SMX), nitrofurantoin and fosfomycin have become alternative first-line antibiotics.
Below are some of the antibiotic classes used most commonly to treat UTIs.
Trimethoprim-Sulfamethoxazole (TMP-SMX)
The typical treatment for an uncomplicated UTI is a 3-day course of the combination drug trimethoprim-sulfamethoxazole, commonly called TMP-SMX (such as Bactrim, Septra, generic). A 1-day course is somewhat less effective but poses a lower risk for side effects. Longer courses (7 - 10 days) work no better than the 3-day course and have a higher rate of side effects.
TMP-SMX should not be used in patients who are allergic to sulfa drugs. Allergic reactions can be very serious. Trimethoprim (such as Proloprim or Trimpex) is sometimes used alone in those allergic to sulfa drugs. TMP-SMX can interfere with the effectiveness of oral contraceptives. High rates of bacterial resistance to TMP-SMX exist in many parts of the United States.
Nitrofurantoin
Nitrofurantoin (Furadantin, Macrodantin, Macrobid, generic) is an antibiotic that is used specifically for urinary tract infections as an alternative to TMP-SMX. It is usually taken twice a day for 5 days. It is not useful for treating kidney infections. Nitrofurantoin frequently causes stomach upset and interacts with many drugs. Other chronic or serious medical conditions may also affect its use. It should not be used in pregnant women within 1 - 2 weeks of delivery, in nursing mothers, or in those with kidney disease.
Fosfomycin
The antibiotic fosfomycin (Monurol) may be prescribed as a 1-dose treatment for women who are pregnant or for other select patients. In general, it is less effective for treating UTIs than TMP-SMX or nitrofurantoin.
Beta-Lactams
The beta-lactam antibiotics share common chemical features and include penicillins, cephalosporins, and some newer similar drugs.
Penicillins. Until recent years, the standard treatment for a UTI was 10 days of amoxicillin, a penicillin antibiotic, but it is now ineffective against E. coli bacteria in many cases. A combination of amoxicillin-clavulanate (Augmentin) is sometimes given for drug-resistant infections.
Cephalosporins. Antibiotics known as cephalosporins are alternatives for infections that do not respond to standard treatments or for special populations. They are often classed as first, second, or third generation. Cephalosporins used for treatment of UTIs include cephalexin (Keflex, generic), cefadroxil (Duricef, generic) cefuroxime (Ceftin, generic),loracarbef (Lorabid), and cefixime (Suprax), among others.
Other Beta-Lactam Drugs. Other beta-lactam antibiotics have been developed. For example, pivmecillinam (a form of mecillinam), is commonly used in Europe for UTIs. It is not available in the United States.
Fluoroquinolones (Quinolones)
Fluoroquinolones (also simply called quinolones) were used as alternatives to TMP-SMX but they are now recommended for UTIs only when other antibiotics are not appropriate. Fluoroquinolones are effective for treating acute kidney infections (pyelonephritis). Examples of quinolones include ofloxacin (Floxacin, generic), ciprofloxacin (Cipro, generic), and levofloxacin (Levaquin, generic). These drugs can have severe side effects that the patient should discuss with the doctor.
Pregnant women should not take fluoroquinolone antibiotics. They also have more adverse effects in children than other antibiotics and should not be the first-line option in most pediatric situations.
Other Antibiotics Used for UTIs
Doripenem. Doripenem (Doribax) is a newer carbapenem antibiotic, which is used to treat complicated urinary tract infections. It is given by injection.
Tetracyclines. Tetracyclines include doxycycline, tetracycline, and minocycline. They may be used for UTIs caused by Mycoplasma or Chlamydia. Side effects include skin reactions to sunlight and tooth discoloration. Tetracyclines cannot be taken by children or pregnant women.
Aminoglycosides. Aminoglycosides (gentamicin, tobramycin, amikacin) are given by injection for very serious bacterial infections. They can be given only in combination with other antibiotics. Gentamicin is the most commonly used aminoglycoside for severe UTIs. They can have very serious side effects, including damage to hearing, sense of balance, and kidneys.
Medications for Treating Symptoms
Although antibiotics can cure most urinary tract infections, severe symptoms can persist for several days until the drug eliminates the bacteria. Other medications may be used for relieving symptoms until the antibiotics take action.
Phenazopyridine. Phenazopyridine (such as Pyridium, Uristat, AZO Standard, Urodol, generic) relieves pain and burning caused by the infection. Patients should not take this medicine for more than 2 days.
Side effects include headache and upset stomach. The drug turns urine a red or orange color, which can stain fabric and be difficult to remove. Rarely, it can cause serious side effects, including shortness of breath, a bluish skin, a sudden reduction in urine output, shortness of breath, and confusion. In such cases, patients should immediately call the doctor.
Antispasm Drugs. Methenamine (Urised, Cystex, generic) or flavoxate (Urispas, generic) reduce bladder spasms, which may occur with some UTIs. These drugs can have severe side effects, however, that the patient should discuss with the doctor.
Lifestyle Changes
Although there is no evidence that good hygiene makes a real difference in preventing UTIs, it is always a wise practice. The following are some hygiene tips for women:
- Clean the genital and urinary areas from front to back with soap and water after each bowel movement.
- Avoid tight-fitting pants.
- Wear cotton-crotch underwear and panty hose, changing both at least once a day. (Mild detergents are best for washing underwear.)
- Take showers rather than baths.
- Avoid bath oils, feminine hygiene sprays, douches, and powders. As a general rule, do not use any product containing perfumes or other possible allergens near the genital area. Douching is never recommended as it may irritate the vagina and urethra and increase the risk of sexually transmitted diseases.
- Choose sanitary napkins instead of tampons (which some doctors believe encourage infection). Napkins and tampons, in any case, should be changed after each urination.
- Drink plenty of fluids and urinate frequently.
Sexual Precautions
Sexual intercourse is one of the most common risk factors for uncomplicated UTIs in women. In addition to abstaining from sex while you have a UTI, the following recommendations may reduce the risks from sexual activity:
- Keep the genital and anal areas clean before and after sex. Urinate before and after intercourse to empty the bladder and cleanse the urethra of bacteria.
- Discuss with your doctor contraceptive alternatives to the spermicides used with condoms and diaphragms. .
- Avoid sex with multiple partners. This can cause many health problems, including sexually transmitted diseases.
Cranberries, Blueberries, and Lignonberries
Cranberries, blueberries, and lignonberry, a European relative of the cranberry, are three fruits that appear to have protective properties against urinary tract infections. These fruits contain compounds called tannins (or proanthocyanadins). Tannins may prevent E. coli bacteria from adhering to cells in the urinary tract, thereby inhibiting infection. Cranberry juice is the best-studied home remedy for UTIs. Many studies have indicated that cranberry juice may help decrease the number of symptomatic UTIs, especially for women with recurrent urinary tract infections.
It is not clear what the optimum dosage is for cranberries, or whether it is best to use juice or tablet form although some studies suggest that drinking juice is more effective than taking tablets. Some research recommends drinking at least 1- 2 cups of cranberry juice daily, or taking at least 300 - 400 mg in tablet form twice daily.
Probiotics and Lactobacilli
Probiotics are beneficial microorganisms that may protect against infections in the genital and urinary tracts. The best-known probiotics are the lactobacilli strains, such as acidophilus, which is found in yogurt and other fermented milk products (kefir), as well as in dietary supplement capsules. The probiotics bifidobacteria and GG lactobacilli may also be helpful. Other probiotics include the lactobacilli rhamnosus, casel, plantarium, bulgaricus, and salivarius, and also Enterococcus faecium and Streptococcus thermophilus. Not all studies show a benefit for probiotics in preventing urinary tract infections. More research is needed.
Resources
- http://kidney.niddk.nih.gov -- National Kidney and Urologic Diseases Clearinghouse
- www.urologyhealth.org -- American Urological Association
- www.acog.org -- American College of Obstetricians and Gynecologists
References
Azzarone G, Liewehr S, O'Connor K. Cystitis. Pediatr Rev. 2007 Dec;28(12):474-6.
Colgan R, Williams M. Diagnosis and treatment of acute uncomplicated cystitis. Am Fam Physician. 2011 Oct 1;84(7):771-6.
Colgan R, Nicolle LE, McGlone A, Hooton TM. Asymptomatic bacteriuria in adults. Am Fam Physician. 2006 Sep 15;74(6):985-90.
Conway PH, Cnaan A, Zaoutis T, Henry BV, Grundmeier RW, Keren R. Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. JAMA. 2007 Jul 11;298(2):179-86
Faust WC, Pohl HG. Role of prophylaxis in vesicoureteral reflux. Curr Opin Urol. 2007 Jul;17(4):252-6.
Foster RT Sr. Uncomplicated urinary tract infections in women. Obstet Gynecol Clin North Am. 2008 Jun;35(2):235-48, viii.
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar;52(5):e103-20.
Gupta K, Trautner B. In the clinic. Urinary tract infection. Ann Intern Med. 2012 Mar 6;156(5):ITC3-1-ITC3-15.
Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012 Mar 15;366(11):1028-37.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010 Mar 1;50(5):625-63.
Jepson RG, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD001321.
Little P, Merriman R, Turner S, Rumsby K, Warner G, Lowes JA, et al. Presentation, pattern, and natural course of severe symptoms, and role of antibiotics and antibiotic resistance among patients presenting with suspected uncomplicated urinary tract infection in primary care: observational study. BMJ. 2010 Feb 5;340:b5633. doi: 10.1136/bmj.b5633.
Little P, Moore MV, Turner S, Rumsby K, Warner G, Lowes JA, et al. Effectiveness of five different approaches in management of urinary tract infection: randomised controlled trial. BMJ. 2010 Feb 5;340:c199. doi: 10.1136/bmj.c199.
Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office, 2007; NIH Publication No. 07-5512.
Montini G, Tullus K, Hewitt I. Febrile urinary tract infections in children. N Engl J Med. 2011 Jul 21;365(3):239-50.
Mori R, Lakhanpaul M, Verrier-Jones K. Diagnosis and management of urinary tract infection in children: summary of NICE guidance. BMJ. 2007 Aug 25;335(7616):395-7.
Peters CA, Skoog SJ, Arant BS Jr, Copp HL, Elder JS, Hudson RG, et al. Summary of the AUA guideline on management of primary vesicoureteral reflux in children. J Urol. 2010 Sep;184(3):1134-44. Epub 2010 Jul 21.
Salo J, Ikäheimo R, Tapiainen T, Uhari M. Childhood urinary tract infections as a cause of chronic kidney disease. Pediatrics. 2011 Nov;128(5):840-7. Epub 2011 Oct 10.
Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management, Roberts KB, Downs SM, Finnell SM, et al. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011 Sep;128(3):595-610. Epub 2011 Aug 28.
U.S. Preventive Services Task Force. Screening for asymptomatic bacteriuria in adults: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2008 Jul 1;149(1):43-7. Ann Intern Med. 2008 Jul 1;149(1):W20-4.
Vazquez JC, Abalos E. Treatments for symptomatic urinary tract infections during pregnancy. Cochrane Database Syst Rev. 2011 Jan 19;(1):CD002256.
Wang CH, Fang CC, Chen NC, Liu SS, Yu PH, Wu TY, et al. Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2012 Jul 9;172(13):988-96.
White B. Diagnosis and treatment of urinary tract infections in children. Am Fam Physician. 2011 Feb 15;83(4):409-15.
|
Review Date:
9/17/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |








