Chronic obstructive pulmonary disease
Highlights
Overview
- Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in the U.S. The disease is characterized by an abnormal inflammatory response in the lungs and restricted airflow (documented by spirometry). The disease typically occurs after age 35.
- Cigarette smoking remains the major cause of COPD, but it isn't the only cause. In most studies, smoking accounts for about 80% of COPD cases. Quitting smoking can improve lung function and help to prevent death from COPD. Other causes, such as genetic syndromes (alpha-1 antitrypsin deficiency) and exposures to pollutants such as dust, irritants and fumes are also involved in the development of the disease.
- An overall treatment strategy may include one or several medications, lifestyle changes, education, pulmonary rehabilitation, oxygen therapy and perhaps surgery.
Medication
- One National Institute of Health (NIH) -funded trial showed that daily azithromycin (plus usual treatment) reduced the frequency of COPD exacerbations and improved quality of life. The long- term effects of taking azithromycin, a broad spectrum antibiotic, are not known. Daily azithromycin is not suitable for patients at risk for abnormal heart rhythms or ear damage.
- The choices among options for inhaled therapy may be based on patient preference, side effects and/or cost. Much research is underway to assess the merits of individual (mono-therapy) vs. combination therapy options, such as these recent findings:
- Alone, tiotropium, a long-acting anticholinergic drug, was found to be significantly better than the beta2-agonist salmeterol in reducing exacerbations in patients with moderate to severe COPD in a one year study.
- Both long-acting beta-agonists (LABA) and inhaled corticosteroids (ICS) yield similar benefits across most outcomes when used as individual therapies. Given their potential side effects, current guidelines support long-acting beta-agonists as primary therapy, supplemented by regular use of corticosteroids for patients who experience frequent exacerbations.
Other Treatments and Guidelines
- Pulmonary rehabilitation may offer a management strategy for patients who experienced a recent exacerbation of COPD. It may reduce hospital admissions and mortality, and improve quality of life.
- In 2009, the American College of Physicians (ACP), American College of Chest Physicians (ACCP), American Thoracic Society (ATS), and European Respiratory Society (ERS), updated its 2007 clinical guidelines on the diagnosis and management of COPD. It stresses the importance of patient history and physical examination for predicting airflow obstruction, spirometry for screening or diagnosis of COPD, and assessing management strategies included inhaled medications, pulmonary rehabilitation and supplemental oxygen.
Introduction
Chronic obstructive pulmonary disease (COPD) is a condition in which there is reduced airflow in the lungs. The disease develops and worsens over time. COPD is not reversible, but therapy can slow its progress.
Although patients can breathe in normally, changes in the small airways cause the tubes to narrow during expiration, making it hard to breathe out. In many patients with COPD, the small sacs where oxygen and carbon dioxide are exchanged are destroyed, gradually depriving the body of enough oxygen.
COPD is associated with a set of breathing-related symptoms:
- Being out of breath, at first when doing physical activities, but as lung function deteriorates, also at rest
- Chronic cough
- Spitting or coughing mucus (phlegm)
The ability to exhale (breathe out) gets worse over time.
The two major diseases in this category are emphysema and chronic bronchitis, both of which are covered in this report. The third, less common disease, is obstructive bronchiolitis, an inflammatory condition of the small airways. Asthma shares some of the same symptoms, but it is a very different disease. People can have asthma and COPD at the same time.
Because smoking is a common cause of both emphysema and chronic bronchitis, these conditions often develop together and frequently require similar treatments and approaches. When chronic bronchitis occurs together with emphysema, it is often difficult for a physician to distinguish between the two diseases.
Emphysema
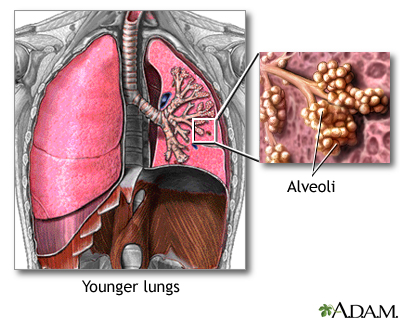
Emphysema is a disease in which the alveoli, grape-like clusters of air sacs at the end of the smallest airways (the bronchioles) are destroyed. It generally takes the following course:
- The walls of the alveoli become inflamed and damaged. Over time they lose the ability to stretch and shrink (elasticity), and pockets of stagnant air (called bullae) form in the injured areas.
- The pockets interfere with the normal working of the lungs by narrowing the airways, trapping air, and making breathing out more difficult.
- The ability to breathe in is not affected. Until the late stages of the disease, oxygen and carbon dioxide levels remain normal.
Chronic Bronchitis
Chronic bronchitis is defined as coughing and excess mucus production that occurs for at least 3 months, during at least 2 consecutive years. In chronic bronchitis, the disease process generally and has the following characteristics:
- Inflammation of the bronchial tubes (from smoking and air pollution) causes the production of mucus, which clogs the airways and makes breathing difficult.
- The mucus is cleared through coughing. Both constant coughing and inflammation can damage the bronchial tubes. The tubes swell and thicken, leaving less room for air flow.
The Lungs
The lungs are two spongy organs surrounded by a thin, moist membrane called the pleura. Each lung is made up of smooth, shiny lobes. The right lung has three lobes, and the left has two. About 90% of the lung is filled with air. Only 10% is solid tissue.
When a person inhales, air travels through the following pathways into the lungs:
- Air is carried from the windpipe (trachea) into the lung through flexible airways called bronchi.
- Like the branches of a tree, bronchi divide into more than a million smaller airways called bronchioles.
- Bronchioles lead to grape-like clusters of microscopic sacs called alveoli.
- In each adult lung there are millions of these tiny alveoli. The thin membrane of the alveoli allows oxygen and carbon dioxide to pass to and from capillaries.
- When the person breathes in deeply, the elastic alveoli unfold and unwind to allow this exchange of gases to occur.
Capillaries, the smallest of the blood vessels, carry blood throughout the body. Red blood cells carry oxygen throughout the body, and return carbon dioxide to the lungs. White blood cells are the critical infection fighters in the body.
Causes
Cigarette smoking is the most important cause of COPD. Cigarette smoke contains irritants that inflame the air passages, setting off a chain of events that damage cells in the lung, increasing the risk for both COPD and lung cancer.
Smoking isn't the only cause of COPD, however. In most studies, smoking accounts for about 80% of cases. Other causes, such as genetic syndromes (alpha-1 antitrypsin deficiency), exposure to pollutants such as dust, irritants and vapors, and asthma are also involved in the development of this disease.
Disease Process
The key process leading to emphysema is not well understood. It appears that inflammatory cells (T lymphocytes, neutrophils, and alveolar macrophages) release chemicals called enzymes that attack the tissue in the deepest part of the lung where oxygen and carbon dioxide are exchanged. As a result, airways become narrowed, breathing out becomes difficult and the vital air sacs themselves are damaged and eventually destroyed.
Smoking
The typical COPD patient is a current or former smoker, over age 50, with a pack-a-day habit of more than 20 years. Lung function continues to get worse as the person ages.
On the positive side, smoking rates in the U.S. are dropping, and the proportion of adults under 55 with COPD is gradually declining. This indicates that the high death rate will eventually level out. In particular, the rate of COPD in young African Americans is declining significantly. The rate in younger Caucasians is not decreasing as dramatically.
The longer a person smokes, the higher the risk for emphysema. Most patients have smoked the equivalent of one pack a year for 20 years, and many have smoked for up to the equivalent of 40 years. Once a smoker quits, the rate of lung function loss becomes the same as in a nonsmoker; however, much of the lung damage that occurred during smoking may not be reversible.
People who smoke both tobacco and marijuana face nearly three times the risk of developing COPD compared to nonsmokers, although smoking marijuana alone does not seem to increase the risk. Researchers say there may be a synergistic effect, in which marijuana increases the susceptibility of the airways to the detrimental effects of tobacco smoke.
Breathing in secondhand smoke may also increase the risk for COPD, because the irritants from cigarette smoke get into the lungs.
Different effects of smoking can lead to emphysema or chronic bronchitis, but smokers generally have signs of both conditions. Emphysema caused by smoking most often occurs in the upper lobes of the lungs.
In chronic bronchitis, smoking triggers inflammation that causes damage in the airways. The processes involved include:
- Damage to the cilia, the hair-like waving projections that move mucus, bacteria, and foreign particles out of the lungs. When cilia are injured, foreign substances become trapped in the lungs and can cause infections that lead to chronic bronchitis.
- Enlargement of the mucus glands in the large airways of the lungs.
- Excess growth of smooth muscle cells in the airway.
Other Exposures
Smoking tobacco is a major risk factor for COPD, yet an estimated 25 - 45% of COPD patients in the developing world have never smoked. In underdeveloped countries, exposure to industrial pollutants in poorly ventilated work areas, and cooking over wood and coal fires (biomass) are also major contributors.
Researchers say exposure to smoke from biomass fires might actually pose the biggest risk for COPD around the world. Other exposures that might increase COPD risk include:
- Dust
- Gases
- Outdoor air pollution
Genetics
Various factors, such as genetic abnormalities, may be necessary for people to develop the airway damage that leads to COPD. The link may be a gene called ADAM33, which researchers have discovered is more common in smokers with COPD than in those who don't have the disease. Other genetic variants linked to the disease have been discovered on chromosome 4, as well as in the gene for the a-nicotinic acetylcholine receptor, CHRNA 3/5 (a chemical messenger that has also been linked to smoking and lung cancer).
Alpha-1 antitrypsin deficiency (A1AD) is the only known genetic risk factor that has been associated with the emphysema type of COPD. About 1% of people with COPD have this disorder, which prevents their bodies from making enough of the protective enzyme, AAT. Without enough AAT, damage occurs in both the walls of the alveoli and the airways leading to them.
Because smoke is a major toxin and deactivates any amounts of AAT that do remain, smokers with AAT deficiency have almost no chance of escaping emphysema. Nonsmokers are also at high risk, however. Emphysema in people with A1AD develops in people as young as 30 years old, who are usually of Northern European descent.
Screening tests are now available to detect the genetic defect that causes A1AD. Couples with a family history of the disease may want to be tested for the deficiency, so they may take protective measures for themselves and any future children they may have. If the condition is already in the family, testing the children is important.
People with AAT who are over age 30, younger patients who have respiratory symptoms, as well as nonsmokers and those with severe and rapidly progressing disease should be screened for COPD each year with lung-function tests.
Other rare genetic conditions have also been suggested as possible causes of COPD in nonsmokers, including cutis laxa, Marfan syndrome, and Ehlers-Danlos syndrome, although these links have not yet been proven.
Bacteria and Viruses
Certain bacteria, particularly Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, are common in the lower airways of nearly half of chronic bronchitis patients.
However, the role of bacteria, viruses, and other organisms in causing chronic symptoms and inflammation is unclear. Some experts believe that a low-level infection in the lungs may trigger an inflammatory reaction that continues to produce acute attacks. Viruses may also exaggerate the lung response to infections, leading to exacerbations of COPD.
Symptoms
The hallmark symptom of COPD is shortness of breath that gets worse over time. It is often accompanied by a phlegm-producing cough and episodes of wheezing. Symptoms may vary, however, or others may be present, depending on the disease involved. Many patients have symptoms of both chronic bronchitis and emphysema.
Symptoms of Emphysema
Typically, the first symptoms of emphysema occur in heavy smokers in their mid-50s:
- The main early symptom is shortness of breath with light physical activity. Coughing is usually minor, and coughs produce little sputum (phlegm).
- Late, severe symptoms include rapid, labored breathing, and persistent craving for air (air hunger), even during rest or after minimal physical activity.
- Patients are often very thin (a wasted look called "cachexia"), have pinkish skin, and tend to breathe through pursed lips.
- Involuntary weight loss and muscle wasting may occur, and can indicate a poor outlook.
Symptoms of alpha-1 antitrypsin-related emphysema tend to appear between the ages of 30 and 40. Like the symptoms of ordinary emphysema, they include:
- Inability to exercise without becoming winded
- Shortness of breath after physical activity
- Wheezing
Symptoms of Chronic Bronchitis
Chronic bronchitis usually causes the following symptoms:
- A chronic cough is the hallmark symptom of chronic bronchitis, even in its early stages. Coughing with excessive phlegm occurs on most days for at least 3 months of the year, during 2 consecutive years. Coughing often starts before shortness of breath.
- Shortness of breath occurs, but it may not be as severe during rest as it is in people with emphysema.
- Lying down at night worsens symptoms in patients with chronic bronchitis and heart failure, so patients must sleep propped up.
- In the late, severe stages of the disease, a lack of oxygen causes the skin to have a blue color (cyanosis).
- The body may swell from fluid build-up caused by heart failure.
Diseases with Similar Symptoms
Several diseases have similar symptoms and may occur with COPD.
Acute Bronchitis
Viruses and bacteria can cause acute bronchitis. In most cases it does not require treatment. The cough typically lasts for 7 - 10 days. In about half of patients, however, coughing can last for up to 3 weeks, and 25% of patients continue to cough for more than 1 month. Patients with severe symptoms may need antibiotics.
Asthma
The classic symptoms of an asthma attack are coughing, wheezing, and shortness of breath (dyspnea). Patients with asthma typically have trouble breathing in and may wheeze when breathing out. People may experience irritation of the nose and throat, thirst, and the need to urinate before an asthma attack begins.
Some people experience chest tightness or pain, or a nonproductive cough that occurs without wheezing. About 75% of patients have chest pain. The pain can be very severe, even if the asthma attack itself is not severe. At the end of an attack, a person will often have a cough that produces a thick, stringy mucus.
People with chronic asthma can get airway obstruction that makes them more likely to develop COPD. However, researchers aren't sure whether people with chronic asthma have symptoms similar to COPD, or if they have COPD itself.
Lung Cancer
Lung cancer does not usually produce symptoms until the disease is advanced. Frequent bouts of pneumonia or a lung infection that does not clear up may be the first signs of lung cancer. Signs of advanced lung cancer may include:
- Bloody phlegm
- Chest pain
- Coughing
- Fever
- Shortness of breath
- Weight loss
Bronchiectasis
Bronchiectasis is an irreversible lung disease in which the walls of the airways in the lung are widened (dilated) and eventually destroyed. Patients with this disease may have chronic sinus infections or inflammation (sinusitis), a chronic cough, and heavy phlegm that often contains blood. People with this condition usually have had serious, frequent respiratory infections, often starting in childhood. Other factors associated with bronchiectasis are:
- Cystic fibrosis
- Problem with the immune system (immunodeficiency)
- Rheumatic diseases
- Smoking
Complications
COPD affects more than 5% of people in the U.S. It is the fourth most common cause of death in the United States, responsible for more than 100,000 deaths each year. Experts predict that it will be the third leading cause of death in the world by 2030 as the population ages and people continue to smoke.
Although COPD has traditionally been considered a man's disease, an increase in women who smoke has caused COPD to skyrocket in women. Women with COPD tend to fare worse than men. They are more likely to be hospitalized and to die from COPD. They also have more severe symptoms, greater depression, and a worse quality of life than men.
Women appear to be more susceptible to the effects of smoking and pollution, possibly because of hormones or other genetic differences. The good news is that women who stop smoking get their lung function back more quickly than men.
The leading cause of death from COPD is respiratory failure. However, patients with mild-to-moderate COPD also tend to develop cardiovascular disease or lung cancer. This likely occurs from inflammation, which is involved in all three diseases.
Traditionally, doctors have measured the severity of COPD by the amount of air that a person can forcibly exhale in one second (FEV1). This amount decreases as COPD gets worse. However, COPD affects other systems and body parts, which provide clues about the severity of the disease. Many physicians now use the BODE index to categorize COPD and predict its outcome. BODE stands for body mass index, degree of airflow obstruction, dyspnea (breathlessness), and exercise capacity as measured in a 6-minute walk test.
Outlook for Patients with Emphysema. If emphysema is detected before it causes symptoms, there may be some chance of reversing it. However, permanent changes in the alveoli usually occur, even in young smokers. Patients with the inherited form of early-onset emphysema are at risk for early death unless the disease is treated and its progression is stopped or slowed. Emphysema patients who have significant, unplanned weight loss (a sign of muscle wasting) have a poorer outlook, regardless of their lung function.
Outlook for Patients with Chronic Bronchitis. Chronic bronchitis does not cause as much lung damage as emphysema, although the airways become blocked by mucus plugs and narrow due to inflammation. Poor air exchange leads to low oxygen levels and high carbon dioxide levels. This poor gas exchange can lead to serious, life-threatening conditions that include severe breathing difficulty and heart failure.
Acute Exacerbations
Acute exacerbations are episodes that occur when the airways suddenly become blocked and symptoms get worse. These events are associated with inflammation in the airways and are generally triggered by an infection in the airway or throughout the body.
Other factors that can trigger serious lung events include:
- Certain medications
- Exposure to irritants in the air (air pollution)
- Seasonal changes (hot weather)
Acute exacerbations include the following symptoms:
- Increased phlegm
- Thicker and darker phlegm
- Shortness of breath (this is the most common and distressing acute symptom)
Acute exacerbations occur, on average, between two and three times a year in patients with moderate-to-severe COPD. They are most often triggered by infections. Smokers have more exacerbations than nonsmokers.
Researchers have discovered that a clot that blocks an artery in the lung (a pulmonary embolus) is present in as many as a quarter of all COPD exacerbations. COPD patients are at higher risk for embolisms than the general public.
Acute exacerbations get better on their own, but they are still the most common cause of hospitalization in COPD patients. Frequent episodes cause lung function to deteriorate quickly. Patients never recover to the condition they were in before the last exacerbation.
Reduced Quality of Life and Mood
Nearly half of COPD patients report some limitation in daily activities. They have trouble walking up stairs or carrying even small packages. Breathing becomes hard work. More than half of patients with COPD have difficulty sleeping (insomnia). Such impairment in quality of life can negatively affect mood.
Those with COPD are more likely to have anxiety, depression, or another psychiatric disorder than people in the general population. Women with COPD are more susceptible to psychological problems than men.
If patients with COPD become anxious or depressed, they may have a poorer outlook than people without emotional problems. Depression and anxiety are associated with an increase in the frequency and length of exacerbations, as well as the number of hospitalizations. Having anxiety can cause exacerbations to last twice as long as they would otherwise. Depression also increases the risk of death in both those with stable COPD and in those with uncontrolled disease. Having depression may prevent people with COPD from eating properly, exercising, taking their medication as prescribed, and getting the medical attention they need.
Low oxygen levels also can impair mental function and short-term memory. Psychological therapy may be particularly helpful for people with COPD.
Malnourishment
People with COPD often have poor nutrition. Patients with chronic bronchitis tend to be obese. Patients with emphysema tend to be underweight. Loss of weight and muscle mass is linked to a poor outcome in COPD. Good nutrition improves the ability to exercise, which in turn builds muscle strength and lung function. Obese patients with COPD who lose weight tend to sleep better.
Heart Disease
Over time, COPD causes low levels of oxygen (hypoxia) and high levels of carbon dioxide (hypercapnia) in the body. In order to boost oxygen delivery, the body compensates in a number of ways:
- Blood vessels in the lung narrow. This leads to high blood pressure in the lungs (pulmonary hypertension).
- More red blood cells are produced to increase the blood's ability to carry oxygen.
- The heart rate increases to pump more blood.
- The breathing rate increases.
Eventually these activities can lead to very serious and even life-threatening conditions:
- Abnormally high blood pressure in the lungs can cause a complication called cor pulmonale. The right ventricle of the heart enlarges, eventually leading to heart failure.
- Chronic bronchitis is associated with a 50% higher risk of death from coronary artery disease, independent of the risks associated with smoking.
- Patients with long-term and severe hypoxia and hypercapnia are at risk for acute respiratory failure, which can cause heart rhythm abnormalities or other life-threatening conditions.
Other Serious Medical Problems Associated with COPD
The smoking that causes COPD is associated with high risks of pneumonia, lung cancer, stroke, and heart attack. Tobacco smoke contains more than 400 substances, many of which are oxidants, metals (such as lead, cadmium, and aluminum), and cancer-causing chemicals (carcinogens). Nicotine itself may not damage tissues, but it addicts smokers to tobacco.
Lung Cancer. Patients with a 30-year history of smoking and signs of limited airflow (most patients with COPD) are at high risk for lung cancer.
Sleep Disturbance. About half of all people with severe COPD experience sleep disorders such as sleep-related hypoxia or insomnia. Nocturnal hypoxia, a lack of oxygen during sleep, occurs when breathing is shallowest during rapid-eye-movement (REM) sleep. It may be due to suppression of the cough reflex and a buildup of mucus. Nocturnal hypoxia is treated with overnight oxygen therapy. As COPD worsens, many patients have trouble falling or staying asleep. COPD patients should not use sleep medications. Nighttime oxygen or a change in COPD medications from beta-agonists to anticholinergics can sometimes help restore restful sleep.
Osteoporosis. Osteoporosis (thin and weakened bones) is a significant problem in patients with COPD. Many conditions associated with COPD, including smoking, lack of vitamin D, sedentary lifestyle, and the use of corticosteroid medications put people at risk for bone density loss and osteoporosis.
Gastroesophageal Reflux (GERD). Many patients with severe COPD have GERD, a condition in which stomach acids back up from the stomach into the esophagus. However, many COPD patients don't report experiencing GERD symptoms such as heartburn.
Aspiration Pneumonia. Problems with breathing and swallowing put people with moderate-to-severe COPD at increased risk for aspiration pneumonia. This condition occurs when saliva, other fluids, or food is breathed into the airways.
Risk Factors
An estimated 64 million people around the world have COPD. In the U.S., about 4.9 million people have emphysema, and 9.9 million have chronic bronchitis. Because emphysema and chronic bronchitis so often occur together, it is difficult to determine the number of emphysema patients versus those with chronic bronchitis. Many patients, even if their symptoms are severe, regard their condition as a natural part of aging, or blame a lack of fitness, and do not get examined by a health care provider.
The main risk factors for COPD include:
- Cigarette smoke
- Age older than 40 years
- Exposure to occupational dust and chemicals
- Exposure to smoke from wood or other biomass fires
- Exposure to indoor air pollution
- Alpha-1 antitrypsin deficiency
Occupational Risk Factors
Workers who are exposed for a long time to toxic chemicals (such as silica or cadmium), industrial smoke, dust, or other air pollutants are at increased risk for COPD. Such workers include:
- Cooks
- Furnace workers
- Grain farmers
- Miners
- Women who cook over open fires
- Railroad workers (from exposure to diesel exhaust)
Allergies and Asthma
Allergens are allergy-causing particles and organisms such as fungi, molds, and house dust. The connection between allergies, asthma, and COPD is the topic of much debate. Some physicians believe allergies and asthma are the early stages of COPD. Another school of thought says that COPD causes changes to the airways that produce asthma symptoms.
Although the exact connection is not known, patients with hyperactive airways due to allergies or asthma are at increased risk for COPD. Patients with COPD who can control their airway problems with bronchodilators (the medication used in asthma) are less likely to die from COPD.
HIV
People infected with HIV are 50 - 60% more likely to develop COPD than people who do not have HIV. The percentage of HIV patients who smoke is not much larger than those who do not smoke. This suggests that HIV itself increases susceptibility to COPD or speeds up the decline in lung function.
Other Risks
Abnormal lung development in the womb might increase the risk for COPD later in life. Researchers have found that newborns with poor airway function are more likely to have breathing disorders as adults. Preventive measures for these children might need to start in infancy.
Research also finds that eating bacon, sausage, and other cured meats might reduce lung function and increase the risk for COPD. Cured meats are high in nitrates, which act much like tobacco smoke to damage the lungs, according to researchers.
Diagnostic Tests
Despite the widespread incidence and seriousness of COPD, studies strongly suggest that it is underdiagnosed, especially in women. Some experts recommend that any adult smoker who complains of a daily cough should be screened for COPD. In one study, nearly half of patients over age 60 who regularly smoked had COPD. Anyone who has a chronic cough, increased phlegm production, or breathing difficulty that gets worse over time should be checked for the disease.
Medical and Personal History
The doctor will request a history that evaluates the patient's risk factors. Risk factors include:
- Past and present smoking
- Exposure to industrial pollutants at work
- Family history of alpha-1 antitrypsin deficiency
- Low exercise capacity (such as trouble climbing stairs or difficulty walking for more than a certain distance)
- Past and present smoking
- History of asthma, allergy, sinusitis, or respiratory infections
Physical Examination
Appearance. There are usually no changes in physical appearance in people with mild-to-moderate COPD. In advanced COPD, patients with emphysema may be wasted and thin, with normal-colored pink skin. Those with chronic bronchitis may have bluish lips and fingers, be obese, and may have swollen feet and legs. Breathing may be rapid and shallow, done through pursed lips, and it may take longer to breathe out.
The patient will be asked to cough and produce phlegm, if possible.
Chest Examination. The physician will next perform a simple examination of the chest area with a stethoscope to listen for:
- Crepitations, a noise resembling a paper bag being rumpled
- Reduced or distant breath sounds
- Signs of pulmonary hypertension
- Wheezing or gurgling sounds
Other findings may include:
- Breathlessness when the patient lies flat
- Increased pressure in the veins
Pulmonary Function Tests (Spirometry)
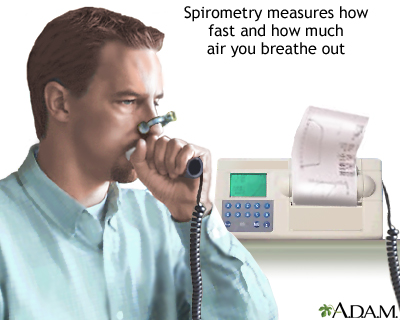
The best tests for diagnosing COPD and seeing how well it responds to treatment are pulmonary function tests. The gold-standard test for patients with respiratory symptoms such as shortness of breath is spirometry. Spirometry measures the volume and force of air as it is exhaled from the lungs. It measures airway obstruction, it can identify COPD early, and the results are standardized so they are always consistent. Because it is easy and reliable, spirometry is an effective method to help health professionals diagnose COPD early, when it is most treatable.
Spirometry is not recommended for screening healthy adults who do not have breathing symptoms. However, it can be used to screen people with a family history of alpha-1 antitrypsin deficiency, or smokers.
During spirometry, the patient is asked to breathe in and breathe out forcefully into an instrument. This is repeated several times. The force of the air is then measured.
From the results, the physician determines two important values.
The forced vital capacity (FVC). FVC is the maximum volume of air that a patient can breathe out with force. It indicates lung size, elasticity, and how well the air passages open and close.
The forced expiratory volume in one second (FEV1). FEV1 is the maximum volume of air that a patient can breathe out in 1 second after breathing in fully. Airflow is considered to be limited if the forced breath out stays low over 1 second. People with COPD have a decline in FEV1 over time. FEV1 is measured as percent of predicted:
- Moderate COPD -- FEV1 50 - 80% of predicted
- Severe COPD -- FEV1 30 - 50% of predicted
- The ratio of FEV1 to FVC (FEV1/FVC) is less than 70% of normal, regardless of whether the patient has an FEV1 greater than 80% or less than 50%
Tests for Measuring the Ability of the Lung to Exchange Oxygen and Carbon Dioxide
Arterial Blood Gas. The physician may request an arterial blood gas test to determine the amount of oxygen and carbon dioxide in the blood (its saturation). Low oxygen (hypoxia) and high carbon dioxide (hypercapnia) levels often indicate chronic bronchitis, but not always emphysema. A blood gas analysis that shows very low oxygen levels is useful for determining which patients would benefit from oxygen therapy. This procedure typically involves drawing blood from an artery in the wrist.
Pulse Oximetry Test. A safe and painless test for measuring oxygen in the blood is called pulse oximetry, which involves placing a probe on the finger or ear lobe. The probe emits two different lights. The amount of each light the blood absorbs is related to how much oxygen the red blood cells carry. This test measures only oxygen in the blood, however, and not carbon dioxide. Results should be taken together with other tests to determine the need for medication or oxygen therapy.
Carbon Monoxide Diffusing Capacity. The lung carbon monoxide diffusing capacity (DLCO) test determines how effectively gases are exchanged between the blood and airways in the lungs. Patients should not eat or exercise before the test, and they should not have smoked for 24 hours.
The patient inhales a mixture of carbon monoxide, helium, and oxygen and holds his or her breath for about 10 seconds. The gas levels are then analyzed from the exhaled breath. Results can help physicians differentiate emphysema from chronic bronchitis and asthma. Patients with emphysema have lower DLCO results (a reduced ability to take up oxygen). The results of this test are also important in helping to determine appropriate candidates for lung reduction surgery. Carbon monoxide levels that are 20% or less than predicted values pose a very high risk for poor survival.
Exhaled Breath. The measurement of nitric oxide (NO) in exhaled breath can be a simple method of diagnosing COPD and monitoring the effects of treatment. In most patients with COPD, no levels are below normal. Levels above normal in a patient with COPD indicate that the person also has asthma.
Imaging Tests
Chest X-Rays. Chest x-rays are often performed, but they are not very useful for detecting early COPD. By the time an x-ray reveals COPD, the patient is already well aware of the condition. X-rays can look for growths in the lungs, and can help rule out other diseases, such as tuberculosis, however.
Clear signs of COPD on x-ray include the following:
- Abnormally large amounts of air spaces in the lung
- A flattened diaphragm
- A smaller heart (however, if the person has heart failure, the heart becomes enlarged and there may not be signs of overinflated lungs)
- Exaggerated lung inflation in upper areas
- Larger amounts of air in the lower lungs in patients with emphysema related to alpha-1 antitrypsin deficiency
Chest x-rays are rarely useful for diagnosing chronic bronchitis, although they sometimes show mild scarring and thickened airway walls.
Computed Tomography. Computed tomography (CT) scans can accurately assess the severity of COPD and may be used to determine the size of the air pockets (bullae) in the lungs.
Other Tests for COPD
Noninvasive Methods for Determining Severity. Questionnaires and short exercise tests are very useful for determining the severity of COPD.
Test for alpha-1 antitrypsin deficiency. Physicians will typically test for the enzyme alpha-1 antitrypsin in COPD patients who are nonsmokers and in people who develop COPD symptoms before age 45.
Additional Blood and Sputum Tests. Additional tests may be required if the physician suspects other medical problems. If the person has pneumonia, for instance, blood and sputum tests and cultures may be performed to determine the cause of infection.
Bronchodilator Challenge. Using a bronchodilator can usually relieve the symptoms of asthma. However, patients with COPD typically have a limited response to bronchodilation. A bronchodilator challenge test may help distinguish between the two diseases. Some patients with COPD experience limited and temporary improvement in FEV1 30 - 45 minutes after inhaling medication from a metered dose inhaler. However, their airflow remains poor.
Treatment
The appropriate medications for COPD depend on its stage of severity, which is determined by the symptoms. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has proposed a strategy that is widely accepted. GOLD categorizes COPD severity as follows:
- Stage I: Smoker's cough, little or no shortness of breath, no symptoms of COPD, FEV1 greater than 80% of predicted.
- Stage II: Shortness of breath on exertion, sputum-producing cough, some symptoms of COPD, FEV1 50 - 80% of predicted.
- Stage III: Shortness of breath on mild exertion, FEV1 30 - 50% of predicted.
- Stage IV: Shortness of breath on mild exertion, right heart failure, bluish skin, nails, and lips (cyanosis), FEV1 less than 30% of predicted.
Classification of COPD Severity | |||
GOLD Stages | Symptoms | FEV1 (% predicted) | *FEV1/FVC (%) |
I: Mild | +/- Symptoms +/- Cough/sputum | > 80 | < 70 |
II: Moderate | +/- Symptoms +/- Cough/sputum/breathing difficulty (dyspnea) | 50 - 80 | < 70 |
III: Severe | +/- Symptoms +/- Cough/sputum/dyspnea | 30 - 50 | < 70 |
IV: Very Severe | Cough/sputum/dyspnea +/- Respiratory failure +/- Right heart failure | < 30 Or respiratory failure Or right heart failure | < 70 |
*Note: FVC -- Forced vital capacity: the maximum volume of air that you can forcibly breathe out from the lungs.FEV1 -- Forced expiratory volume in 1 second: the amount of air you can breathe out during the first second after you take your deepest breath. | |||
The American College of Physicians has issued revised guidelines for COPD treatment, which include:
- In patients with stable COPD, reserve treatment for those who have respiratory symptoms and FEV1 of less than 60% of predicted.
- Patients with symptoms and FEV1 of less than 60% of predicted should be treated with long-acting inhaled beta-agonists, long-acting inhaled anticholinergics, or inhaled corticosteroids. Combination inhaled therapies may be used in these patients.
- Patients with COPD and resting hypoxia should be treated with oxygen therapy.
- Patients with symptoms and FEV1 of less than 50% of predicted should consider pulmonary rehabilitation.
Treatment Approach for Stable COPD
Stopping Smoking. Stopping smoking is the first and most important step in treating COPD and slowing its progression. Quitting smoking decreases symptoms of breathlessness and cough, as well as the risk of heart disease, likely due to decreased inflammation.
Diet. Good nutrition is always important. Dietary issues become critical in late COPD, when breathing is difficult. Many patients with COPD lose muscle tone and body mass, and appear to waste away. This may be due to the extreme effort it takes to breathe, which rapidly consumes calories. Some patients find it difficult to stop the effort of breathing long enough to chew food. A nutritionist can find the right foods and design meal plans to help COPD patients be as healthy as possible. There is not strong evidence to support the use of nutritional supplements in patients with COPD. It may help to avoid cured meats, which research indicates can increase the risk of COPD.
Supplemental Oxygen. Supplemental oxygen is an important part of COPD therapy. It can:
- Improve exercise endurance
- Improve quality of life and mental outlook
- Improve sleep
- Reduce breathlessness
- Reduce pulmonary hypertension
Supplemental oxygen affects all of these factors, along with the lungs' ability to exchange carbon dioxide for oxygen. There is some evidence that supplemental oxygen may also reduce heart problems in patients with COPD. Long-term oxygen therapy given continuously through the nose has been shown to extend survival by as much as 30%.
Pulmonary Rehabilitation. Pulmonary rehabilitation is a proven method of relieving shortness of breath (dyspnea), reducing hospitalizations and disability from COPD, increasing exercise capacity, and improving mental and physical quality of life, although there is no proof that it improves survival. This treatment is recommended for patients with stable chronic lung disease who are significantly affected by respiratory symptoms. Although pulmonary rehabilitation doesn't improve lung function, it strengthens muscles and improves other body systems to minimize the effects of lung dysfunction.
Many hospitals offer these programs, which are led by a team of health professionals. Pulmonary rehabilitation can also be done in the home or community. The treatment is tailored to individual patients, but it usually includes:
- Breathing training
- Disease education
- Exercise (endurance and resistance training)
- Nutritional advice
- Psychological assessment
Patients are usually assessed at the beginning and end of the program. Programs generally last 6 - 12 weeks, but longer programs appear to provide more long-term benefits. In one study, an 8-week pulmonary rehabilitation program reduced the number of COPD patients admitted to the hospital by 46%. Maintenance programs may slightly improve long-term outcomes.
Exercise. Exercise is important for maintaining strength and endurance, both of which are greatly affected by COPD. Weight-bearing exercises are important for maintaining quality of life and the ability to live independently. For the greatest benefit, programs should combine low- and high-intensity exercise with strength and endurance training. The use of noninvasive ventilation (NIPPV) during exercise provides some small, very short-term benefit. Receiving supplemental oxygen during rehabilitative exercise may improve patients' endurance. There is no evidence that inspiratory muscle training (training the muscles used to breathe in) is effective during pulmonary rehabilitation.
Surgery. When a patient no longer responds to medications, surgery becomes a possible option. Choices include:
- Bullectomy
- Lung transplantation
- Lung volume reduction surgery (LVRS)
Treating COPD in Older Adults. Older adults are at greater risk for complications or death from COPD, and their treatment needs to be tailored accordingly. Treatment in this group includes short- and long-acting bronchodilators, vaccines, and quitting smoking.
General Guidelines for Treating Acute Exacerbations
The goal of COPD treatment, in addition to providing symptom relief, is to prevent exacerbations. Each exacerbation causes lung function to decline. Bringing lung function back to its pre-exacerbation state can take 6 months. When exacerbations are frequent, lung function may never return to normal, and the patient's condition spirals downward.
Exacerbations are most commonly caused by bacterial or viral infections, or by air pollution. The cause is never identified in about one-third of patients.
Treatment of exacerbations commonly includes the following measures:
Oxygen. Supplemental oxygen with controlled oxygen therapy and noninvasive positive pressure ventilation.
Bronchodilators. Inhaled anticholinergics or short-acting beta2-agonists may be used. Theophylline is not recommended, because it provides very little benefit and carries a risk of serious side effects.
Corticosteroids. Corticosteroid medications may be given either through a vein (intravenously) or by mouth (orally), for up to 2 weeks. This treatment is only possible in patients who have not received long-term oral corticosteroid therapy.
Antibiotics. These may be used if there are signs of infection, such as fever or yellow or green phlegm.
Medications
Anticholinergic Medications
Anticholinergic medications relax the bronchial muscles and open up the airways. Opening up the airways is called bronchodilation. Bronchodilators do not change the overall course of the disease. However, these medications help improve breathlessness, the ability to exercise, and quality of life.
Brands and Benefits. Anticholinergics used for COPD include short-acting ipratropium (Atrovent) and long-acting tiotropium (Spiriva). They are considered standard maintenance medications for COPD.
A single inhaler containing both ipratropium and the common beta2-agonist albuterol (Combivent) may be more effective than either medication alone.
Long-acting anticholinergic medications are also being given along with inhaled corticosteroids and long-acting beta-agonists. Although the combination may not reduce the number of exacerbations, it improves lung function and quality of life, and it reduces hospitalizations. For patients who experience frequent symptoms of COPD, current guidelines support long-acting beta-agonists as primary therapy for COPD, supplemented by regular use of inhaled corticosteroids.
Side Effects. Anticholinergics have few severe side effects, and they are less likely to interfere with sleep than the other standard inhaled medications. Side effects include mild cough and dry mouth. Anticholinergics should be used cautiously in people with glaucoma or an enlarged prostate.
Beta2-Agonists
When anticholinergics are no longer enough -- and sometimes in place of an anticholinergic medication -- health care providers will prescribe a beta2-agonist. GOLD guidelines recommend that all patients with COPD stages II - IV take a long-acting beta2-agonist.
Short-Acting Beta2-agonists. For patients whose symptoms come and go, such as with exertion, short-acting bronchodilators are recommended. Albuterol (Proventil, Ventolin) is the standard short-acting beta2-agonist. Others include:
- Fenoteral
- Levalbuterol hydrocholoride (Xopenex)
- Levalbuterol tartrate (Xopenex HFA)
- Pirbuterol (Maxair)
There is no evidence that one beta2-agonist is better than another. Newer beta2-agonists, including levalbuterol (Xopenex), have more specific actions than the older medications. Most are inhaled and are effective for 3 - 6 hours.
Long-Acting Beta2-Agonists. Long-acting bronchodilators are more effective than short-acting bronchodilators for patients with more significant long-term symptoms. Long-acting beta2-agonists salmeterol (Serevent) and formoterol (Foradil) are proving to be particularly effective as long-term maintenance therapy for COPD. They reduce exacerbations by 20 - 25%, they may help prevent bacteria from building up on the airways, and they may offer real improvements in lung function. A nebulized formulation of formoterol is also available for the treatment of COPD.
Some inhalers combine a long-acting beta2-agonist and a corticosteroid (such as Advair, Seretide, and Symbicort). Combining a corticosteroid and long-acting beta2-agonist may reduce exacerbations and improve lung function, but it can also increase the risk of pneumonia.
Side Effects. Side effects of both long- and short-acting beta2-agonists include anxiety, tremor, restlessness, and headaches. Patients may experience fast and irregular heartbeats. A physician should be notified immediately if such side effects occur, particularly in people with existing heart conditions. Such patients face an increased risk of sudden death from heart-related causes. This risk is higher with medications taken by mouth or through nebulizers, but there have also been reports of heart attacks and chest pain (angina) in some patients using inhaled beta2-agonists.
Loss of Effectiveness and Overdose. All long-acting beta2-agonists come with a boxed warning about an increased risk of asthma-related deaths, but there is no evidence that people who have COPD without asthma are at increased risk.
There has been some concern that short-acting beta2-agonists may become less effective when taken regularly over time. A major concern is that patients who perceive beta2-agonists as being less effective may overuse them. Overdose can be serious and, in rare cases, even life threatening, particularly in patients with heart disease or asthma.
Corticosteroids
Corticosteroids are powerful anti-inflammatory drugs.
Oral Corticosteroids. Oral corticosteroids are reserved for treating COPD exacerbations, and research finds that they are better than inhaled corticosteroids for this purpose. They speed the time to recovery and reduce the length of the hospital stay, but they do not reduce mortality or affect the long-term progression of the disease. They shouldn't be regularly used for stable disease because of the increased risk of side effects.
Oral corticosteroids are recommended for the initial treatment of patients who are hospitalized for COPD exacerbations, yet research finds that most patients are given IV steroids instead.
Inhaled Corticosteroids. Inhaled corticosteroids (ICS) are the mainstay of asthma therapy. However, their primary use in COPD is to treat exacerbations, rather than for long term maintenance.
A review of evidence has shown that both long-acting beta-agonists (LABA) and inhaled corticosteroids (ICS) yield similar benefits for COPD patients when used as individual therapies. However, long-acting beta-agonists are slightly better at improving lung function, and ICS are slightly more effective at improving quality of life, but increase the risk of pneumonia. Therefore, current guidelines support long-acting beta-agonists as primary therapy, supplemented by regular use of corticosteroids for patients who experience frequent exacerbations.
Theophylline and Other Methylxanthines
Methylxanthines (primarily slow-release theophylline) are also bronchodilators, which relax the airways of the lungs. These drugs are used in patients with more severe exacerbations that do not respond completely to corticosteroids, oxygen, or antibiotics.
These drugs do not significantly improve lung function, symptoms, or overall outcomes when used for acute exacerbations. Some experts believe that the modest benefits do not outweigh the risk of toxic side effects from these drugs. Side effects are generally related to the amount of theophylline in the blood. At high doses, side effects can include nausea, anxiety, headaches, insomnia, vomiting, irregular heartbeat, tremors, and seizures.
Administering Inhaled Drugs
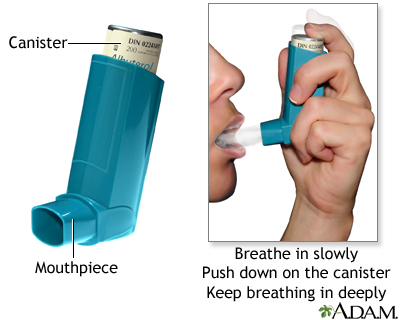
Many COPD drugs are inhaled using metered dose inhalers, dry powder inhalers, or nebulizers.
Metered-Dose Inhaler. The standard device for delivering COPD medication is the metered-dose inhaler (MDI). This device allows precise doses to be delivered directly to the lungs. A holding chamber, or spacer, improves delivery by giving the patient more time to inhale the medication.
Breath-Activated Dry Powder Inhalers. Dry powder inhalers (DPIs) deliver a powdered form of the drug directly into the lungs. DPIs are as effective as MDIs and are easier to manage, especially for older adults. Humidity or extreme temperatures can affect DPI performance, so these devices should not be stored in humid places (such as bathroom cabinets) or in locations with high temperatures (such as car glove compartments during the summer months).
Other Handheld Inhalers. Respimat delivers a fine-mist spray that is created by forcing the liquid medication through nozzles. It does not use any propellant.
Nebulizers. A nebulizer is a device that administers the drug in a fine spray that the patient breathes in. Nebulizers are often used in hospitals or when the patient cannot use an inhaler.
Medicines That Loosen Lung Secretions
Patients with persistent coughing and phlegm often use medications that loosen secretions and help move them out of the lungs.
Expectorants. Expectorants, such as guaifenesin (found in common cough remedies), stimulate the flow of fluid in the airways and help move secretions using the motion of cilia (the hair-like structures in the lung) and coughing. Expectorants have not been shown to benefit patients with COPD.
Mucolytics. Mucolytics contain ingredients that make thick phlegm more watery and easier to cough up. Although mucolytics are not generally recommended for people with COPD, there is some evidence that they may reduce exacerbations by a small amount in some patient with moderate-to-severe COPD who take these
medications throughout the winter. The most effective mucolytic is stopping smoking. Anticholinergics appear to decrease the production of mucus. Beta2-agonists and theophylline improve mucus clearance.
Other Medications
Statins. The same drugs used to lower cholesterol may also help protect the lungs of COPD patients, in part due to their anti-inflammatory effects. However, more research is needed to prove these benefits, and to determine the optimal statin dose for COPD patients.
Alpha-1 Antitrypsin Augmentation Therapy. Some patients with alpha-1 antitrypsin deficiency are treated with weekly intravenous infusions of alpha-1 antitrypsin. Research finds that this therapy can't be recommended for COPD patients with alpha-1 antitrypsin deficiency, because the treatment is expensive and there is not enough evidence to show that it reduces exacerbations or improves lung function.
Antibiotics
Treating Acute Bronchitis or Pneumonia in COPD Patients. People with COPD are at increased risk for pneumonia, but any lung infection can worsen symptoms and speed deterioration of lung function. Patients with acute bronchitis or pneumonia who have signs of bacterial infection, such as green or yellow phlegm, usually need antibiotics.
Streptococcus pneumoniae, Haemophilus influenzae, and Moxarella catarrhalis are the most common causes of pneumonia or exacerbations in people with COPD. The choice of antibiotic depends on the bacteria being treated and bacterial resistance to common antibiotics in the area. Giving preventive antibiotics to patients with frequent exacerbations is not recommended because this practice contributes to the development of bacterial resistance.
Antibiotic Options
Beta-Lactams
Beta-lactam antibiotics include penicillins, cephalosporins, and some newer medications. They share common chemical features, and all interfere with bacterial cell walls.
Penicillins. Penicillin was the first antibiotic. Many forms of this still-important drug are available today:
- Penicillin derivatives called aminopenicillins, particularly amoxicillin (Amoxil, Polymox, Trimox, Wymox, or any generic formulation), are now the most common penicillins used. Amoxicillin is inexpensive, and at one time it was highly effective against S. pneumoniae. Unfortunately, bacterial resistance to amoxicillin has increased significantly, both among S. pneumoniae and H. influenzae. Ampicillin is similar, but it requires more doses and has more severe gastrointestinal side effects than amoxicillin.
- Amoxicillin-clavulanate (Augmentin) is known as an augmented penicillin. It works against a wide spectrum of bacteria and is used for more severe exacerbations. An extended-release form is also available.
Many people have a history of allergic reaction to penicillin, but some evidence suggests the allergy may not return in a significant number of adults. Skin tests are available to help determine whether someone with a history of penicillin allergies could tolerate these important antibiotics.
Cephalosporins. Most of these antibiotics are not very effective against bacteria that have developed resistance to penicillin, and they are only used for more severe exacerbations. They are classified according to their generation:
- Second generation: cefaclor (Ceclor), cefuroxime (Ceftin), cefprozil (Cefzil), and loracarbef (Lorabid)
- Third generation: cefpodoxime (Vantin), cefdinir (Omnicef), cefditoren (Spectracef), cefixime (Suprax), and ceftibuten (Cedex). Ceftriaxone (Rocephin) is an injected cephalosporin. These antibiotics are effective against a wide range of Gram-negative bacteria, and some are also able to treat penicillin-resistant S. pneumoniae infections.
Fluoroquinolones (Quinolones)
Fluoroquinolones ("quinolones") interfere with the bacteria's genetic material to prevent them from reproducing. These antibiotics are used for more severe exacerbations.
- "Respiratory quinolones" are currently the most effective drugs available against a wide range of bacteria. These drugs include levofloxacin (Levaquin) and gemifloxacin (Factive). Levofloxacin was the first drug approved specifically for penicillin-resistant S. pneumoniae. Some of the newer fluoroquinolones need to be taken only once a day.
- The fourth-generation quinolones moxifloxacin (Avelox) and clinafloxacin (which is still in development) are proving effective against anaerobic bacteria.
S. pneumoniae strains that are resistant to the respiratory quinolones are uncommon in the U.S., but resistance is increasing.
Many quinolones cause side effects, including sensitivity to light and nervous system (neurologic), psychiatric, and heart problems. Pregnant women should not take this class of drugs. Quinolones also enhance the potency of oral anti-clotting drugs.
When it comes to treating acute exacerbations of chronic bronchitis, so-called second-line antibiotics (amoxicillin, clavulanate, macrolides, second- or third-generation cephalosporines, and quinolones) appear to be more effective than -- and just as safe as -- first-generation antibiotics (ampicillin, doxycycline, and trimethoprim/sulfamethoxazole).
Macrolides and Azalides
Macrolides and azalides also affect the genetics of bacteria. These drugs include:
- Azithromycin (Zithromax, Zmax)
- Clarithromycin (Biaxin)
- Erythromycin
- Roxithromycin (Rulid)
These antibiotics are effective against atypical bacteria such as mycoplasma and chlamydia. All but erythromycin are effective against H. influenzae. Macrolides and azalides are also used in some cases for S. pneumoniae and M. catarrhalis, but there is increasing bacterial resistance to these medicines. One National Institute of Health (NIH) funded trial showed that daily azithromycin (plus usual treatment) reduced the frequency of COPD exacerbations and improved quality of life. However, mild hearing loss was more common in patients taking azithromycin, and long-term use may not be suitable for patients at risk of heart rhythm disturbances. The implications of these results for practice are still not known.
Tetracyclines
Tetracyclines inhibit the growth of bacteria. They include doxycycline, tetracycline, and minocycline. They can be effective against S. pneumoniae and M. catarrhalis, but bacteria that are resistant to penicillin are also often resistant to doxycycline. The side effects of tetracyclines include skin reactions to sunlight, burning in the throat, and tooth discoloration.
Trimethoprim-Sulfamethoxazole
Trimethoprim-sulfamethoxazole (Bactrim, Cotrim, and Septra) is less expensive than amoxicillin and is particularly useful for adults with mild bacterial upper respiratory infections who are allergic to penicillin. The drug is no longer effective against certain streptococcal strains. It should not be used in patients whose infections occur after dental work, or in people who are allergic to sulfa drugs. Allergic reactions can be very serious.
Oxygen-Replacement Therapy
Lung function may eventually worsen to the point that patients need supplemental oxygen delivered through portable or stationary tanks.
Continuous Therapy. Continuous oxygen therapy (more than 15 hours a day) is the only treatment for emphysema that has been proven to prolong survival in certain patients. It also improves alertness, motor speed, and hand strength. Continuous oxygen therapy is usually recommended for patients with:
- Lung oxygen level below 55 mm Hg while resting
- Lung oxygen level below 60 mm Hg while resting, plus right heart failure or an abnormal increase in red blood cells
Supplemental oxygen may also benefit patients with moderately low blood oxygen levels, but more research needs to be done to confirm this.
Ideally, patients should receive enough oxygen to keep the oxygen level at 65 mm HG, but no less than 60 mm HG, or at an oxygen saturation level of at least 90%. Patients may need extra oxygen flow during sleep or physical activity.
About 40% of patients improve enough in 1 month to stop continuous treatment, although these patients should be observed closely. COPD often gets worse, and patients need to restart oxygen therapy. Some patients get worse in spite of treatment, although it is not possible to predict who is at risk for oxygen therapy failure. The addition of nitric oxide, a gas that widens blood vessels, may offer additional benefits.
Intermittent Oxygen. Patients with less severe COPD who are not on permanent oxygen maintenance may need supplemental oxygen during specific circumstances:
- Patients whose oxygen level drops below 55 mm HG only while exercising may benefit from supplemental oxygen during physical activity. Supplemental oxygen may improve endurance, and it enhances the delivery of oxygen to the muscles while they are working.
- Patients whose oxygen level drops below 55 mm HG during sleep may need oxygen at night. Such patients usually experience fitful, poor-quality sleep. This type of oxygen therapy does not appear to affect survival or prolong the time until patients need continuous oxygen therapy.
Oxygen During Travel. People on continuous oxygen therapy who are traveling by plane should increase their oxygen by 1 - 2 liters per minute during the trip. People on intermittent oxygen therapy may need oxygen during air travel if the trip is longer than 2 hours and they develop symptoms, or if they experience a drop in oxygen levels before traveling. People are not allowed to bring their own oxygen tanks on board an airplane; many airlines will provide oxygen if notified 48 - 72 hours in advance. It is important to note that aircraft cabins are pressurized to the equivalent of 8,000 feet above sea level. Such pressures could be potentially dangerous for people with severe COPD.
Oxygen Storage and Delivery Systems
Unless they are bed-bound, patients usually use a combination of stationary and mobile oxygen systems.
Stationary Systems. The most common stationary oxygen system is the concentrator, an electrical device that pulls oxygen from the air. It weighs about 35 pounds and cannot be battery operated, so a patient can use it only at home.
Portable Units. Portable units containing electronic oxygen-conserving devices weigh only a few pounds and can provide up to 8 hours of oxygen. Some portable units weigh 6.5 lbs, with liquid oxygen supplies that last 4 hours. Some weigh 9.5 lbs, with an oxygen supply that lasts 8 hours when used at a flow rate of 2 liters per minute.
Compressed or Liquid Oxygen. Oxygen can be administered from large stationary tanks or small portable ones, either as compressed gas or liquid oxygen. A container of liquid oxygen lasts four times longer than compressed gas of the same weight, and it is easier to fill. Liquid oxygen is very beneficial for patients who want to maintain an active life, although the tanks require occasional venting to release pressure, and this wastes oxygen. They are also more expensive.
Precautions. Supplemental oxygen is a fire hazard, and some hotels and residences do not allow its use. No one should smoke near an oxygen tank, and tanks should be stored safely, secured to a wall and away from heaters and furnaces.
Devices for Administering Oxygen
Oxygen is usually administered in one of three ways: through a nasal canula, transtracheal catheter, or electronic demand device.
Nasal Canula. Using a nasal canula, oxygen is delivered through a long, thin plastic tube that runs from the oxygen tank to small plastic prongs that fit in the nostrils. The tube can be very long when attached to a stationary tank in order to accommodate walking throughout a house, or relatively short when attached to a portable unit.
A reservoir pouch is a recent innovation added to this device that provides an extra rush of oxygen when a patient starts to inhale. This method is inexpensive and easy to use, but some patients are embarrassed by its appearance under their noses.
Transtracheal Oxygen. Transtracheal oxygen is delivered directly into the windpipe (trachea) through a catheter tube implanted by a surgeon. The device is inconspicuous, and patients are very likely to use it. Long-term complications may include infection, dislodgment, and blockage by mucus, which can be very serious. Complications of the procedure itself occur in 3 - 5% of cases and can include lung spasms and uncontrollable coughing.
Electronic Demand Devices. Electronic devices that sense the beginning of a breath and deliver a pulse of oxygen are also available, although they are complicated, expensive, and have a risk for mechanical failure. Newer units have a continuous flow bypass switch that allows oxygen to still be delivered if the battery runs down.
Devices to Assist Breathing
In emergency situations, oxygen may be delivered to the patient in various ways.
Noninvasive Positive Pressure Ventilation (NPPV). If the patient is able to breathe naturally, oxygen is delivered through a tube using a tightly fitted oxygen mask to maintain airway pressure during breathing. Some physicians now believe such devices should be first-line treatments (in addition to medications) for managing respiratory failure after an acute exacerbation. NPPV allows the patient to talk and drink fluids, and is much easier to tolerate than nose or throat tubes. It cannot be used on patients with rapidly deteriorating COPD, those who are uncooperative, or those who have a facial shape that does not allow the mask to seal tightly.
Intubation. When standard oxygen therapy does not meet a patient's needs, endotracheal intubation may be required to deliver high concentrations of oxygen. With intubation, a tube is inserted down through either the nose or the mouth, and oxygen is given through the tube.
Mechanical Ventilation. In very serious cases such as acute respiratory failure, a mechanical ventilator can be used to take over the function of breathing. The primary goal of ventilation is to remove carbon dioxide and restore a balanced exchange of gases.
Most patients have a low tolerance for intubation, and the tubes are often removed early due to discomfort. Patients with these tubes may need painkillers, sedatives, or muscle relaxants.
There are also several complications that lead to the removal of breathing tubes:
- Bleeding
- Ejection of the tube after coughing
- Mucus plugs
Some preliminary evidence suggests that IV corticosteroid use in patients with COPD on mechanical ventilation may reduce the length of time mechanical ventilation is needed and improve the success of noninvasive mechanical ventilation.
Lifestyle Changes
Quitting Smoking and Avoiding Other Irritants
Quitting smoking is the first and most essential step in treating COPD and slowing its progress. In many people who quit early, lung function stabilizes and eventually declines to about the rate of nonsmokers in the same age group. In some people, lung function may even improve slightly after quitting. As COPD progresses, quitting smoking can slow the rate of decline; however, lost lung function is never fully recovered.
Most patients who smoke try to quit an average of seven times before they are successful. Using a combination of smoking cessation aids improves the likelihood of quitting. These include nicotine replacement products (such as patches, gum, nasal spray, and lozenges), counseling, and prescription medications such as bupropion (Zyban) and varenicline (Chantix).
Preventing Upper Respiratory Infections
Good Hygiene. People should wash their hands with ordinary soap before eating and after going outside the home. Antibacterial soaps add little protection, particularly against viruses.
Vaccines. Two important vaccinations are recommended to protect against respiratory infection.
- Seasonal influenza vaccination. People with COPD should be vaccinated against influenza each year at least 6 weeks before flu season begins. Flu shots appear to help reduce exacerbations of COPD during flu season.
- Pneumococcal vaccine. The adult-type pneumococcal vaccine protects against 23 types of pneumococcus, a common cause of pneumonia. Everyone with COPD should have this vaccine at least once. Patients who had their first shot more than 5 years previously may benefit from a booster vaccine. The vaccine remains effective for years. Flu and pneumococcal vaccines can be given at the same time without increasing side effects.
Breathing Exercises
Pursed-Lip Breathing. A technique called pursed-lip breathing can help improve a patient's lung function before starting activities or doing a strenuous task, such as heavy lifting. Pursed-lip breathing helps change pressure in the airways and prevents the small airways from collapsing. To use this technique:
- First, inhale through the nose, moving the abdominal muscles outward so that the diaphragm lowers and the lungs fill with air.
- Exhale through the mouth with the lips pursed, making a hissing sound.
- Take twice as long breathing out as you did breathing in, so that there is pressure in the windpipe and chest, and trapped air is forced out.
Holding Breath and Coughing. A simple technique is to inhale deeply and slowly, hold the breath for 5 - 10 seconds, then cough while breathing out.
Controlling Secretions
Fluids and Humidity. Patients with congestion and heavy phlegm should drink plenty of fluids and keep their homes humidified.
Chest Therapy. Chest therapy involves breathing in rhythmically for three to four deep breaths, then coughing to produce phlegm. Tapping the chest may also help loosen and bring up phlegm in patients who produce a lot of it. Avoid chest therapy during an acute exacerbation of COPD.
When coughing to produce mucus, another method is to lean forward and "huff" repeatedly. Take relaxed breaths, and then huff again. Avoid forceful coughing, if possible.
Physical Exercise
Because COPD is not simply a lung condition, but a disease that causes wasting of the muscles and bones, certain physical exercises may be very helpful.
Strengthening Exercises for the Limbs. Exercising and strengthening the muscles in the arms and legs helps some patients improve their endurance and reduce breathlessness. These exercises may also help with everyday activities, like climbing stairs and standing up from a chair. Exercising only one leg at a time (for example, pedaling a stationary bicycle with one leg instead of two) might benefit patients who are usually too out-of-breath to exercise, and help them increase their exercise capacity.
Walking. Walking is the best exercise for patients with emphysema. In studies of lung rehabilitation, regular exercise increased walking distance and improved breathing. Patients should try to walk three or four times a day for 5 - 15 minutes each time. Devices that assist with breathing may reduce the breathlessness that occurs during exercise.
Yoga and Eastern Practices. Yoga and tai chi, two practices that use deep breathing and meditation techniques, may be particularly beneficial for COPD patients. Research is underway to determine whether yoga is helpful for COPD patients.
Dietary Factors
Because many patients with chronic bronchitis are obese and many with emphysema are underweight, nutrition assessment is an important part of COPD treatment. Not getting enough of foods that are rich in vitamins A, C, and E, and having a lack of fruits and vegetables can contribute to the development of the disease.
Protein and Fats. Patients with body wasting (cachexia) lack enough protein. Although most healthy diets emphasize proteins from fish, poultry, and lean meat, these people may benefit from foods with a higher-than-average fat content. (People should still prefer healthy fats, however, such as those found in olive oil and oily fish.)
Fruits, Vegetables, and Whole Grains. Healthy foods are as important for lung function as they are for general health. Specific foods that may be important for healthy lungs are those that contain antioxidants (fresh, deep green and yellow-orange fruits and vegetables), selenium (fish, nuts, red meat, grains, eggs, chicken, liver, and garlic), plant chemicals called flavonoids (apples, onions), and magnesium (green leafy vegetables, nuts, whole grains, milk, and meats). One study found that, compared to a Mediterranean diet, which is high in fruits, vegetables, and whole grains, a Western diet high in red meat and simple carbohydrates increased the risk of COPD fivefold.
Vitamin supplements are not helpful, and they may be very harmful for smokers.
Air Travel
Patients with COPD must take extra precautions when traveling by plane. High altitudes may worsen breathing problems and reduce blood oxygen . Air travel can almost always be managed, but additional pre-assessment medical testing, planning and expense may be required. It is best to discuss the following with your physician before flight travel:
- Current control of symptoms
- Previous travel experience
- Time since the last episode of COPD symptoms
Patients will need to arrange for some services in advance, such as in-flight oxygen or wheelchairs and they may need to notify the airline of certain medications, ventilators or continuous positive airway pressure (CPAP) machines. COPD patients may consider obtaining a frequent traveler’s medical card (FREMEC).
Air travel should be avoided in patients who have:
- Infectious tuberculosis
- Ongoing pneumothorax with persistent air leak
- Major haemoptysis
Usual oxygen requirement at sea level at a flow rate exceeding 41/min.
Psychological Support
Patients with COPD are at high risk for depression and anxiety, which can impair their outlook on life. Depression often gets worse as people with COPD need to limit their activities and social interactions. Psychological counseling and social support are important for helping people improve their emotional state, cope with daily stresses, and maintain their independence and social relationships.
Minimizing Airborne Contaminants
As much as possible, patients should avoid exposure to airborne irritants, including:
- Aerosol products
- Hair sprays
- Insecticides
- Paint sprayers
- Smoke from wood fires
To minimize the amount of contaminants in the home:
- Avoid exposure to pollen, pet dander, house dust, and mold.
- Eliminate molds and mildew from household water damage.
- Have furnaces and chimneys inspected and cleaned periodically.
- Make sure wood-burning stoves or fireplaces are well ventilated and meet the Environmental Protection Agency's safety standards. Burn only pressed wood products labeled "exterior grade," because they contain the fewest pollutants.
- Ventilate by keeping windows open (weather permitting), using exhaust fans for stoves and vents for furnaces, and keeping fireplace flues open.
Surgical Procedures
Surgery -- as a last resort -- may help some patients with very severe COPD. Coverage for such procedures varies among insurance carriers. A major drawback is that patients must be in good enough health to undergo major surgery. By the time COPD is advanced, however, this is usually not the case. As a result, surgery cannot help most COPD patients.
The three available surgical options that are appropriate for some patients with COPD are lung transplantation, lung-volume reduction surgery, and bullectomy.
Lung Transplantation
Three-year survival rates after lung transplantation are about 60% for patients with emphysema or alpha-1 antitrypsin deficiency. Patients may have a transplant of one lung, both lungs, or the lungs plus the heart. The increasingly long waiting time for donor organs and the extraordinary expense are both obstacles to this procedure.
Candidates. The best candidates are under age 65 and have severe heart and lung disease, with a life expectancy of less than 18 months. However, lung transplantation is becoming more out of favor for patients with end-stage COPD because it is unclear whether it provides a "useful" quality of life.
Waiting Time. Up to one-third of patients awaiting lung transplantation die before a suitable donor is available. There were more than 1,600 lung transplant operations performed in the United States in 2010, according to the Organ Procurement and Transplantation Network. As of this writing, nearly 1,800 people were waiting for a new lung.
The United Network for Organ Sharing (UNOS) assigns lungs for transplants based on an allocation score, rather than time spent on the waiting list. The allocation score takes into account the length of time a patient is likely to survive before and after a transplant. This policy applies to transplant candidates who are age 12 or older.
Complications. Transplant patients must take drugs that suppress the immune system to prevent the body from rejecting the transplanted organ. Nevertheless, rejection is the primary cause of complications and death. The mortality rate from the procedure itself is about 10%.
Outcomes. About 38% of lung transplants involve both lungs. Transplanting both lungs as opposed to just one significantly improves survival rates in patients under age 60. The average survival in patients who have both lungs transplanted is 6.41 years, compared to 4.59 years in patients with a single-lung transplant.
Lung Volume-Reduction Surgery
In lung volume-reduction surgery (LVRS), more than 30% of severely diseased lung tissue is removed, and the remaining parts of the lung are joined together. Breathing improvements after surgery are mainly due to the following factors:
- Improvement in the ability of the lung and chest wall to spring back during breathing
- Improvement in the function of the muscles, such as the diaphragm, involved with breathing
Prognosis. The largest study to-date, called the National Emphysema Treatment Trial (NETT), compared surgery to medical therapy. This study found that patients whose emphysema was in the upper lobes of the lungs and who had poor exercise ability (poor lung function) before surgery were more likely to benefit from surgery. These benefits included an increased chance of being alive 5 years after the surgery, an improved exercise ability, fewer symptoms, and a better quality of life.
In successful cases, the improvement is most notable within the first 6 months, after which the condition begins to get worse again. After 3 years, lung function deteriorates to the same level as it was before the procedure. LVRS is substantially more expensive than medical treatment.
Possible Candidates. The procedure is used only in people with severe emphysema, and in some people who have alpha-1 antitrypsin deficiency. It is not used for those with chronic bronchitis. Appropriate candidates with alpha-1 antitrypsin deficiency (even if they have disease in the lower lobe) may do well, but the procedure is only useful in a minority of these patients. Candidates must have the following characteristics:
- Under age 75
- Poor lung function (FEV1 less than 40% but higher than 20% of predicted)
- Carbon monoxide diffusing capacity of more than 20% of predicted
- Hyperinflated lungs (total lung capacity greater than 120% of predicted), generally with involvement of the upper lungs
One year after surgery, lung transplant recipients have much better lung function, greater exercise capacity, and less breathlessness than LVRS patients. However, they are less likely to survive, and the transplant is far more expensive than LVRS.
Patients may not qualify for LVRS if they have:
- Chest wall deformity
- Dependence on corticosteroids
- Psychological problems
- Recent tobacco, drug, or alcohol dependence
- Scarring around the membrane of the lung
- Severe medical conditions that limit their lifespan
Other indicators of a poor outlook include severe lung complications and air pockets in diseased areas of the lungs (bullae).
Specific Techniques. At this time, the preferred technique is surgery done on both lungs (bilateral lung volume reduction). Surgeons use either an open approach, making a large cut in the chest area, or video-assisted thoracoscopy (VATS), which is less invasive and involves several small cuts. Either method is effective and has similar complication rates. Lines of staples are typically used to reduce lung volume.
The alternative technique is surgery done on only one lung (unilateral lung volume reduction). Some centers believe this approach may cause fewer complications and the benefits last longer, although not all evidence supports its use over the bilateral method.
Bullectomy
Another option for COPD is bullectomy, in which giant air pockets and surrounding lung tissue are removed. It is generally limited to patients with giant bullae (not the typical COPD patient) and those with alpha-1 antitrypsin deficiency.
Resources
- www.lungusa.org -- American Lung Association
- www.nhlbi.nih.gov -- National Heart, Lung, and Blood Institute
- www.aarc.org -- American Association for Respiratory Care
- www.njc.org -- National Jewish Medical and Research Center
- www.alpha1.org -- Alpha1 National Association
- www.emphysemafoundation.org -- The National Emphysema Foundation
- www.thoracic.org -- American Thoracic Society
- www.sts.org -- Society of Thoracic Surgeons
- www.unos.org -- United Network for Organ Sharing
- www.copd-international.com -- COPD International (patient support site)
References
Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Inhaled corticosteroids vs. placebo for preventing COPD exacerbations: a systematic review and meta-regression of randomized controlled trials. Chest. 2010. 137(2):318-325.
Ahmedzai S, Balfour-Lynn IM, Bewick T, et al; British Thoracic Society Standards of Care Committee. Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax.
2011 Sep;66 Suppl 1:i1-30.
Albert RK, Connett J, Bailey WC, Casaburi R, et al; COPD Clinical Research Network. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011;365(8):689-98.
Alía I, de la Cal MA, Esteban A, et al. Efficacy of corticosteroid therapy in patients with an acute exacerbation of
chronic obstructive pulmonary disease receiving ventilatory support. Arch Intern Med. 2011;171(21):1939-46.
Casaburi R, ZuWallack R. Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. NEJM. 2009;360(13):1329-1335.
Celli BR, Thomas NE, Anderson JA, Ferguson GT, Jenkins CR, Jones PW, et al. Effect of pharmacotherapy on rate of decline of lung function in chronic obstructive pulmonary disease: results from the TORCH study. Am J Respir Crit Care Med. 2008;178:332-338.
De Voogd JN, Wempe JB, Koëter GH, Postema K, van Sonderen E, Ranchor AV, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009/135:619-625.
Drugs for chronic obstructive pulmonary disease. Treat Guidel Med Lett. 2010;8(99):83-88; quiz 89-90.
Eisner MD, Anthonisen N, Coultas D, Kuenzli N, Perez-Padilla R, Postma D, et al. An official American Thoracic Society public policy statement: Novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182(5):693-718.
Global Initiative for Chronic Obstructive Lung Disease. Pocket Guide to COPD Diagnosis, Management, and Prevention. 2010.
Gooneratne NS, Patel NP, Corcoran A. Chronic obstructive pulmonary disease diagnosis and management in older adults. J Am Geriatr Soc. 2010;58(6):1153-1162.
Gøtzsche PC, Johansen HK. Intravenous alpha-1 antitrypsin augmentation therapy for treating patients with alpha-1 antitrypsin deficiency and lung disease. Cochrane Database Syst Rev. 2010 Jul 7;(7):CD007851.
Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128-1138.
Janda S, Park K, FitzGerald JM, Elminan M, Swiston J. Statins in COPD: A systematic review. Chest. 2009;136(3):734-743.
Lapperre TS, Snoeck-Stroband JB, Gosman MME, Jansen DF, van Schadewijk A, Thiadens HA, et a. Effect of fluticasone with and without salmeterol on pulmonary outcomes in chronic obstructive pulmonary disease. Ann Intern Med. 2009:151(8):517-527.
Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Bejamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA. 2010;303(23):2359-2367.
Littner MR. In the clinic. Chronic obstructive pulmonary disease. Ann InternMed. 2011;154(7):ITC4-1-ITC4-15; quiz ITC4-16. Review.
Poole P, Black PN. Mucolytic agents for chronic bronchitis or chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006 Jul 19;3:CD001287.
Puhan MA, Gimeno-Santos E, Scharplatz M, Troosters T, Walters EH, Steurer J. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;(10):CD005305.Review.
Qaseem A, Wilt TJ, Weinberger SE, et al; American College of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-91.
Rabe KF. Anticholinergic drugs for the treatment of COPD are safe...are they? Chest. 2010. 137(1):1-3.
Rizkallah J, Man SF, Sin DD. Prevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2009;135:786-793.
Rodrigo G, Castro-Rodriguez JA, Plaza V. Safety and efficacy of combined long-acting beta-agonists and inhaled corticosteroids vs. long-acting beta-agonists monotherapy for stable COPD: a systematic review. Chest. 2009; 136(4):1029-1038.
Salvi S, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374(9691):733-743.
Silverman EK, Sandhaus RA. Alpha 1-antitrypsin deficiency. NEJM. 2009;360:2749-2757.
Sin DD, Tashkin D, Zhang X, Radner F, Sjöbring U, Thorén A, et al. Budesonide and the risk of pneumonia: a meta-analysis of individual patient data. Lancet. 2009;374(9691):712-719.
Soriano JB, Zielinski J, Price D. Screening for and early detection of chronic obstructive pulmonary disease. Lancet. 2009;374(9691):721-732.
Spencer S, Karner C, Cates CJ, Evans DJ. Inhaled corticosteroids versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;12:CD007033. Review.
Stoller JK, Panos RJ, Krachman S, Doherty DE, Make B. Long-Term Oxygen Treatment Trial Research Group. Oxygen therapy for patients with COPD: current evidence and the long-term oxygen treatment trial. Chest. 2010;138(1):179-187.
Thabut G, Christie JD, Ravaud P, Castier Y, Brugière O, Fournier M, et al. Survival after bilateral versus single lung transplantation for patients with chronic obstructive pulmonary disease: a retrospective analysis of registry data. Lancet. 2008;371:744-751.
U.S. Preventive Services Task Force. Screening for Chronic Obstructive Pulmonary Disease Using Spirometry: Recommendation Statement. Am Fam Physician. 2009;80(8):853-854.
Vogelmeier C, Hederer B, Glaab T, et al; POET-COPD Investigators. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011;364(12):1093-1103.
Welsh EJ, Cates CJ, Poole P. Combination inhaled steroid and long-acting beta2-agonist versus tiotropium for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2010 May 12;(5):CD007891.
|
Review Date:
5/15/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |







