Uterine fibroids and hysterectomy
Highlights
Uterine Fibroids
Uterine fibroids, also called leimyomas or myomas, are non-cancerous growths that originate in the muscular wall of the uterus. Fibroids are the most common type of tumor found in female reproductive organs. Uterine fibroids are very common, especially among African-American women.
Symptoms of Uterine Fibroids
Common symptoms of uterine fibroids may include:
- Heavy and prolonged menstrual bleeding
- Pressure and pain in the abdomen and lower back
- Frequent urination
- Constipation
- Pain during intercourse
- Some women with fibroids do not have any symptoms
Complications of Uterine Fibroids
- Fibroids can increase pregnancy complications and delivery risks.
- Anemia due to iron deficiency may result from heavy menstrual bleeding.
- Large fibroids may reduce fertility, although this is not very common.
Treatment
Many women with fibroids choose not to have treatment, especially if they are approaching the age of menopause. Fibroids grow slowly and usually shrink after menopause. Treatment includes various drug and surgical options.
Medications for Fibroids
- Continuous-dosing oral contraceptives can reduce or eliminate menstrual periods.
- Progestin-releasing intrauterine devices can help control excessive menstrual bleeding (menorrhagia). The levonorgestrel-releasing intrauterine system (Mirena) is approved by the Food and Drug Administration (FDA) for treatment of menorrhagia.
- Gonadotropin-releasing hormone (GnRH) agonists reduce estrogen and progesterone levels, which diminishes the size of fibroids.
Surgical Options
Invasive and less-invasive surgical methods include:
- Myomectomy
- Uterine artery embolization
- Endometrial ablation
- Magnetic resonance-guided focused ultrasound (still not commonly available)
- Hysterectomy
Introduction
A uterine fibroid (known medically as a leiomyoma or myoma) is a noncancerous (benign) growth of smooth muscle and connective tissue. Fibroids can range in size from as small as a pinhead to larger than a melon. Fibroids have been reported weighing more than 20 pounds.
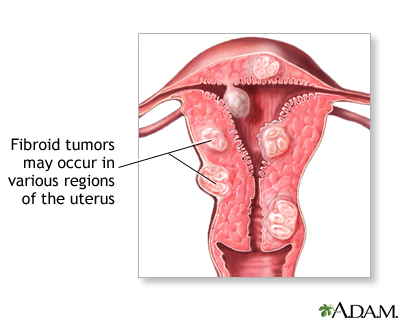
Fibroids originate from the thick wall of the uterus and are categorized by where they grow:
- Intramural fibroids grow within the middle and thickest layer of the uterus (called the myometrium).
- Subserosal fibroids grow out from the thin outer fibrous layer of the uterus (called the serosa). Subserosal can be either stalk-like (pedunculated) or broad-based (sessile).
- Submucosal fibroids grow from the uterine wall toward and into the inner lining of the uterus (the endometrium). Submucosal fibroids can also be stalk-like or broad-based.
The Female Reproductive System
The primary structures in the reproductive system are as follows:
- The uterus is a pear-shaped organ located between the bladder and lower intestine. It consists of two parts, the body and the cervix.
- When a woman is not pregnant the body of the uterus is about the size of a fist, with its walls pressed against each other. During pregnancy the walls of the uterus are pushed apart as the fetus grows.
- The cervix is the lower portion of the uterus. It has a canal opening into the vagina with an opening called the os, which allows menstrual blood to flow out of the uterus into the vagina.
- Leading off each side of the body of the uterus are two tubes known as the fallopian tubes. Near the end of each tube is an ovary.
- Ovaries are egg-producing organs that hold 200,000 - 400,000 follicles (from folliculus, meaning "sack" in Latin). These cellular sacks contain the materials needed to produce ripened eggs, or ova.
The inner lining of the uterus is called the endometrium. During pregnancy this inner lining thickens and becomes enriched with blood vessels to house and support the growing fetus. If pregnancy does not occur, the endometrium is shed as part of the menstrual flow. Menstrual flow also consists of blood and mucus from the cervix and vagina.
Reproductive Hormones. The hypothalamus (an area in the brain) and the pituitary gland regulate the reproductive hormones. The pituitary gland is often referred to as the master gland because of its important role in many vital functions, many of which require hormones.
In women, six key hormones serve as chemical messengers that regulate the reproductive system:
- The hypothalamus first releases the gonadotropin-releasing hormone (GnRH).
- This chemical, in turn, stimulates the pituitary gland to produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- Estrogen, progesterone, and the male hormone testosterone are secreted by the ovaries at the command of FSH and LH and complete the hormonal group necessary for reproductive health.
It is not clear what causes fibroids, but estrogen and progesterone appear to play a role in their growth. Fibroids tend to shrink after menopause, when estrogen levels decline.
Risk Factors
Uterine fibroids are the most common tumor found in female reproductive organs.
Age
Fibroids are most common in women from their 30s through early 50s. (After menopause, fibroids tend to shrink.) About 20 - 40% of women age 35 and older have fibroids of significant enough size to cause symptoms.
Race and Ethnicity
Uterine fibroids are particularly common in African-American women, and these women tend to develop them at a younger age than white women.
Family History
Family history (having a mother or sister who had fibroids) may increase risk.
Other Possible Risk Factors
Obesity and high blood pressure may possibly be associated with increased fibroid risk
Complications
Effect on Fertility
Most fibroids appear to have only a small effect on a woman’s fertility. Female infertility is usually due to other factors than fibroids.
Effect on Pregnancy
Fibroids may increase pregnancy complications and delivery risks. These may include:
- Cesarean section delivery
- Breech presentation (baby enters the birth canal upside down with feet or buttocks emerging first)
- Preterm birth
- Placenta previa (placenta covers the cervix)
- Excessive bleeding after giving birth (postpartum hemorrhage)
Anemia
Anemia due to iron deficiency can develop if fibroids cause excessive bleeding. Oddly enough, smaller fibroids, usually submucosal, are more likely to cause abnormally heavy bleeding than larger ones.
Most cases of anemia are mild and can be treated with dietary changes and iron supplements. However, prolonged and severe anemia that is not treated can cause heart problems.
Urinary Tract Infection
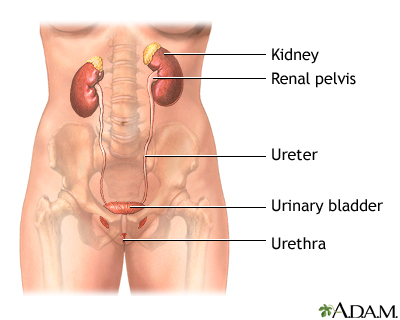
Large fibroids that press against the bladder occasionally result in urinary tract infections. Pressure on the ureters may cause urinary obstruction and kidney damage.
Uterine Cancer
Fibroids are nearly always noncancerous, even if they contain cells with abnormal shapes. Cancer of the uterus usually develops in the lining of the uterus (endometrial cancer). Only in rare cases (less than 0.1%) does cancer develop from a malignant change in a fibroid (called leiomyosarcoma). Nevertheless, rapidly enlarging fibroids in a premenopausal woman or even slowly enlarging fibroids in a postmenopausal woman need evaluation to rule out cancer.
Symptoms
Many patients with fibroids do not have symptoms. When they do, symptoms may include:
- Heavy Menstrual Bleeding. The most common symptom is prolonged and heavy bleeding during menstruation. This is caused by fibroid growth bordering the uterine cavity. Menstrual periods may also last longer than normal.
- Menstrual Pain. Heavy bleeding and clots can cause severe cramping and pain during menstrual periods.
- Abdominal Pressure and Pain. Large fibroids can cause pressure and pain in the abdomen or lower back that sometimes feels like menstrual cramps
- Abdominal and Uterine Enlargement. As the fibroids grow larger, some women feel them as hard lumps in the lower abdomen. Very large fibroids may give the abdomen the appearance of pregnancy and cause a feeling of heaviness and pressure. In fact, large fibroids are defined by comparing the size of the uterus to the size it would be at specific months during gestation.
- Pain During Intercourse. Fibroids can cause pain during sexual intercourse (dyspareunia).
- Urinary Problems. Large fibroids may press against the bladder and urinary tract and cause frequent urination or the urge to urinate, particularly when a woman is lying down at night. Fibroids pressing on the ureters (the tubes going from the kidneys to the bladder) may obstruct or block the flow of urine.
- Constipation. Fibroid pressure against the rectum can cause constipation.
Diagnosis
Pelvic Exam and Medical History
Doctors can detect some fibroids as masses (lumps) during a pelvic exam. During a pelvic exam, the doctor will check for pregnancy-related conditions and other conditions, such as ovarian cysts. The doctor will ask you about your medical history, particularly as it relates to menstrual bleeding patterns. Other causes of abnormal uterine bleeding must also be considered.
Ultrasound
Ultrasound is the standard imaging technique for detecting uterine fibroids. The doctor will order transabdominal and transvaginal ultrasounds. Ultrasound is a painless technique that uses sound waves to image the uterus and ovaries. In transabdominal ultrasound, the ultrasound probe is moved over the abdominal area. In transvaginal ultrasound, the probe is inserted into the vagina.
A variation of ultrasound, called hysterosonography, uses ultrasound along with saline (salt water) infused into the uterus to enhance the visualization of the uterus.
Hysteroscopy
Hysteroscopy is a procedure that may be used to detect the presence of fibroids, polyps, or other causes of bleeding. (It may also be used during surgical procedures to remove fibroids.)
Hysteroscopy can be performed in a doctor’s office or in a hospital setting. The procedure uses a long flexible tube called a hysteroscope, which is inserted into the vagina and through the cervix to reach the uterus. A fiber-optic light source and a tiny camera in the tube allow the doctor to view the cavity. The uterus is filled with saline or carbon dioxide to inflate the cavity and provide better viewing. This can cause cramping.
Hysteroscopy is non-invasive and does not require incisions; however, some women report severe pain with the procedure. Local, regional, or general anesthesia may be given.
Laparoscopy
In some cases, laparoscopic surgery may be performed as a diagnostic procedure. Laparoscopy involves inserting a fiber-optic scope into a small incision made near the navel. Whereas hysteroscopy allows the doctor to view inside the uterus, laparoscopy provides a view of the outside of the uterus, including the ovaries, fallopian tubes, and general pelvic area.
Other Tests
In certain cases, the doctor may perform an endometrial biopsy to determine if there are abnormal cells in the lining of the uterus that suggest cancer. Endometrial biopsy can be performed in a doctor's office, with or without anesthesia. Dilation & curettage (D&C) is a more invasive procedure that involves scraping the inside lining of the uterus. It can be used to take tissue samples and also as a procedure to help temporarily reduce heavy menstrual bleeding.
The doctor may also order a complete blood count (CBC) to check for signs of anemia.
Ruling out Other Conditions that Cause Heavy Bleeding
Almost all women, at some time in their reproductive life, experience heavy bleeding during menstrual periods.
A number of conditions can cause or contribute to the risk:
- Menstrual disorders
- Miscarriage
- Having late periods or approaching menopause
- Uterine polyps (small benign growths in the uterus)
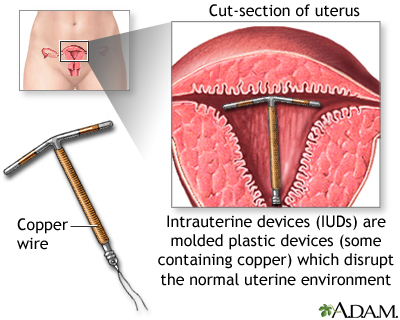
- Intrauterine device (IUD)
- Bleeding disorders that impair blood clotting, Von Willebrand disease
- Uterine cancer
- Pelvic infections
- Adenomyosis. This condition occurs when glands from the uterine lining become embedded in the uterine muscle. Its symptoms are nearly identical to fibroids (heavy bleeding and pain).
- Medical conditions, including thyroid problems and systemic lupus erythematosus
- Certain drugs, including anticoagulants and anti-inflammatory medications.
- Often, the cause of heavy bleeding is unknown.
Treatment
Many women with uterine fibroids do not require treatment. A woman’s age and the severity of her symptoms are important factors in considering treatment options.
The three treatment options are:
- Watchful Waiting. A woman may choose to delay having any treatment, particularly if she is close to reaching menopause. Periodic pelvic exams and ultrasounds can help track the progression of her fibroid condition.
- Drug Therapy. Hormonal treatments such as oral contraceptives or a progestin-releasing IUD can help reduce heavy bleeding and pain. Gonadotropin releasing hormone (GnRH) agonists stop ovulation and the production of estrogen, and can reduce fibroid size.
- Surgery. There are many surgical options ranging from less invasive to very invasive. They include removal of the fibroid (myomectomy), removal of the endometrial lining (endometrial ablation), shrinking the blood supply to the fibroid (uterine artery embolization), and removal of the uterus (hysterectomy).
Women should discuss each option with their doctor. Deciding on a particular surgical procedure depends on the location, size, and number of fibroids. Certain procedures affect a woman's fertility and are recommended only for women who are past childbearing age or who do not want to become pregnant. In terms of surgical options, myomectomy is generally the only commonly performed procedure that preserves fertility.
Medications
For fibroid pain relief, women can use acetaminophen (Tylenol, generic) or nonsteroidal anti-inflammatory drugs (NSAIDS) such as ibuprofen (Motrin, Advil, generic) or naproxen (Aleve, generic).
Prescription drug treatment of fibroids uses medicines that block or suppress estrogen, progesterone, or both hormones.
Hormonal Contraceptives
Oral contraceptives (OCs) are sometimes used to control the heavy menstrual bleeding associated with fibroids, but they do not reduce fibroid growth. Newer types of continuous-dosing OCs reduce or eliminate the number of periods a woman has per year.
Intrauterine devices (IUDs) that release progestin can be very beneficial for reducing heavy bleeding. Specifically, the levonorgestrel-releasing intrauterine system, or LNG-IUS (Mirena), has shown excellent results. It is approved by the FDA to treat heavy menstrual bleeding. Many doctors now recommend the LNG-IUS as a first-line treatment for heavy menstrual bleeding, particularly for women who may face hysterectomy (removal of uterus).
GnRH Agonists
Gonadotropin-releasing hormone (GnRH) agonists include the implant goserelin (Zoladex), a monthly injection of leuprolide (Lupron Depot, generic), and the nasal spray nafarelin (Synarel). GnRH agonists block the release of the reproductive hormones LH (luteinizing hormone) and FSH (follicle-stimulating hormone). As a result, the ovaries stop ovulating and producing estrogen. Basically, GnRH agonists induce a temporary menopause.
GnRH agonists may be used as drug treatment to shrink fibroids in women who are approaching the age of menopause. They may also be used as a preoperative treatment 3 - 4 months before fibroid surgery to reduce fibroid size so that a more minimally invasive surgical procedure can be performed.
Before using these drugs, the doctor should be certain that no other complicating conditions are present, particularly leiomyosarcoma (cancer). The use of these drugs can delay treatment of the malignancy and cause severe complications.
Commonly reported side effects, which can be severe in some women, include menopausal-like symptoms. These symptoms include hot flashes, night sweats, vaginal dryness, weight gain, and depression. The side effects vary in intensity, depending on the GnRH agonist. They may be more intense with leuprolide and persist after the drug has been stopped.
The most important concern is possible osteoporosis from estrogen loss. Women should not take these drugs for more than 6 months.
GnRH treatments used alone do not prevent pregnancy. Furthermore, if a woman becomes pregnant during their use, there is some risk for birth defects.
Surgical Alternatives to Hysterectomy
Myomectomy
A myomectomy surgically removes only the fibroids and leaves the uterus intact, often preserving fertility. Myomectomy may also help regulate abnormal uterine bleeding caused by fibroids. Not all women are candidates for myomectomy. If the fibroids are numerous or large, myomectomy can become complicated, resulting in increased blood loss. If cancer is found, conversion to a full hysterectomy may be necessary.
To perform a myomectomy, the surgeon may use a standard "open" surgical approach (laparotomy) or less invasive ones (hysteroscopy or laparoscopy).
- Laparotomy. Laparotomy uses a normal abdominal incision and conventional "open" surgery. It is used for subserosal or intramural fibroids that are very large (usually more than 4 inches), that are numerous, or when cancer is suspected. While complete recovery takes less than a week with laparoscopy and hysteroscopy, recovery from a standard abdominal myomectomy takes as long as 6 - 8 weeks. Open laparotomy poses a higher risk for scarring and blood loss than with the less invasive procedures, a concern for women who want to retain fertility.
- Hysteroscopy. A hysteroscopic myomectomy may be used for submucosal fibroids found in the uterine cavity. With this procedure, fibroids are removed using an instrument called a hysteroscopic resectoscope, which is passed up into the uterine cavity through the vagina and cervical canal. The doctor then uses an electrosurgical wire loop to surgically remove (resect) the fibroid.
- Laparoscopy. Women whose uterus is no larger than it would be at a 6-week pregnancy and who have a small number of subserosal fibroids may be eligible for treatment with laparoscopy. As with hysteroscopy, thin scopes are used that contain surgical and viewing instruments. Laparoscopy requires only tiny incisions, and has a much faster recovery time than laparotomy.
Complications. The risks for myomectomy are generally the same of those for other surgical procedures, including bleeding and infection.
Recurrence of Fibroids. Myomectomy is not necessarily a permanent solution for fibroids. They can recur after these procedures.
Uterine Artery Embolization
Uterine artery embolization (UAE), also called uterine fibroid embolization (UFE), is a relatively new way of treating fibroids. UAE deprives fibroids of their blood supply, causing them to shrink. UAE is a minimally invasive radiology treatment and is technically a nonsurgical therapy. It is much less invasive than hysterectomy and myomectomy, and involves a shorter recovery time than the other procedures. The patient remains conscious, although sedated, during the procedure, which takes around 60 - 90 minutes.
The procedure is typically performed in the following manner:
- The patient receives a sedative to cause drowsiness, and a local anesthetic is applied to the skin around the groin.
- An interventional radiologist makes a small quarter-inch incision in the skin and inserts a catheter (a thin tube) into the femoral artery. The femoral artery is a large artery that begins in the lower abdomen and extends down to the thigh. The radiologist then threads the catheter into the uterine artery.
- Small plastic particles are injected into the artery. These particles block the blood supply to the tiny arteries that feed fibroid cells, and the tissue eventually dies.
- Patients usually stay in the hospital overnight after UAE and are given pain medication. Pelvic cramps are common for the first 24 hours after the procedure.
- It takes 1 - 2 weeks for the patient to recover from the procedure and return to work. It may take several months to several years for the fibroids to completely shrink.
- Most patients have a light, brownish color vaginal discharge for several days following UAE, which may last until the next menstrual cycle. Most women resume regular menstrual cycles within 2 - 3 months of the procedure. Heavy menstrual bleeding reduced by the second or third cycle.
Effect on Fertility. In general, UAE is considered an option for only those who have completed childbearing. The American College of Obstetricians and Gynecologists advises women who wish to have children that it is not yet known how this procedure affects their potential for becoming pregnant. Some evidence indicates UAE may increase the risk for miscarriage in women who do become pregnant.
Complications. UAE has a lower rate of complication than hysterectomy and laparotic myomectomy and a shorter hospital stay. Compared to other procedures, women who have UAE miss fewer days of work. Serious complications occur in fewer than 0.5% of cases. In addition to potential impact on fertility, other postoperative effects may include.
- Pain. Abdominal cramps and pelvic pain after the procedure are nearly universal and may be intense. Pain usually begins soon after the procedure and typically plateaus by 6 hours. The pain usually improves each day over the next several days. A low-grade fever and general malaise are also common in the first week after the procedure.
- Early menopause. Most women who have UAE will continue to have normal menstrual periods. Some women, however, go through menopause after the procedure. Menopause is more likely to occur in women over age 45 who have UAE.
Success Rates. Studies on uterine artery embolization show high patient satisfaction (over 90%) and low complication rates. Menorrhagia symptoms, as well as pelvic pain and urinary symptoms, improve in 85 - 95% of patients within 3 months after treatment. Uterine artery embolization is effective for most patients. However, some women may have fibroid recurrence and may need future procedures (repeat embolization or hysterectomy).
Some studies suggest that women with larger single fibroids or larger uteruses are not good candidates for UAE.
Endometrial Ablation
Endometrial ablation destroys the lining of the uterus (the endometrium) and is usually performed to stop heavy menstrual bleeding. It may also be used to treat women with small fibroids. It is not helpful for large fibroids or for fibroids that have grown outside of the interior uterine lining. For most women, this procedure stops the monthly menstrual flow. In some women, menstrual flow is not stopped but is significantly reduced.
Endometrial ablation procedures use some form of heat (radiofrequency, heated fluid, microwave) to destroy the uterine lining. The procedure is typically done on an outpatient basis and can take as few as 10 minutes to perform. Recovery generally takes a few days, although watery or bloody discharge can last for several weeks.
Endometrial ablation significantly decreases the likelihood a woman will become pregnant. However, pregnancy can still occur and this procedure increases the risks of complications, including miscarriage. Women who have this procedure must be committed to not becoming pregnant and to using birth control. A main concern of endometrial ablation is that it may delay or make it more difficult to diagnose uterine cancer in the future.
Magnetic Resonance Guided Focused Ultrasound (MRgFUS)
MRgFUS is a non-invasive procedure that uses high-intensity ultrasound waves to heat and destroy (ablate) uterine fibroids. This “thermal ablation” procedure is performed with a device, the ExAblate, which combines magnetic resonance imaging (MRI) with ultrasound.
During the 3-hour procedure, the patient lies inside an MRI machine. The patient receives a mild sedative to help relax but remains conscious throughout the procedure. The radiologist uses the MRI to target the fibroid tissue and direct the ultrasound beam. The MRI also helps the radiologist monitor the temperature generated by the ultrasound.
MRgFUS is appropriate only for women who have completed childbearing or who do not intend to become pregnant. The procedure cannot treat all types of fibroids. Fibroids that are located near the bowel and bladder, or outside of the imaging area, cannot be treated.
This procedure was approved in 2004, and long-term results are not yet available. Likewise, it requires an extensive period of time involving MRI equipment. Many insurance companies do not pay for this treatment.
Hysterectomy
Hysterectomy is the surgical removal of the uterus. The ovaries may also be removed, although this is not necessary for fibroid treatment. Hysterectomy is a permanent solution for fibroids, and is an option if other treatments have not worked or are not appropriate.
A woman cannot become pregnant after having a hysterectomy. If the ovaries are removed along with the uterus, hysterectomy causes immediate menopause.
Types of Hysterectomies
Once a decision for a hysterectomy has been made, the patient should discuss with her doctor what will be removed. The common choices are:
- Total hysterectomy (removal of uterus and cervix).
- Subototal, also called supracervical hysterectomy (removal of uterus and preservation of the cervix).
- Oophorectomy (removal of an ovary). Bilateral oopherectomy is the removal of both ovaries. Bilateral salpingo-oophorectomy is the removal of the fallopian tubes and ovaries). These procedures can be performed with either total or supracervical hysterectomy.
Types of Hysterectomy Procedures
Hysterectomy procedures include:
- Abdominal hysterectomy
- Vaginal hysterectomy
- Laparoscopically assisted vaginal hysterectomy (LAVH)
- Laparoscopic hysterectomy
- Robotic hysterectomy
Abdominal Hysterectomy. Abdominal hysterectomy is the standard procedure. It is best suited for women with large fibroids, when the ovaries need to be removed, or when cancer or pelvic disease is present. The surgeon makes a 5-inch to 7-inch incision in the lower part of the belly. The cut may either be vertical, or it may go horizontally across the abdomen, just above the pubic hair (a bikini cut). The bikini cut incision heals faster and is less noticeable than a vertical incision, which is used in more complicated cases. The patient may need to remain in the hospital for 3 - 4 days, and recuperation at home takes about 4 - 6 weeks.
Vaginal Hysterectomy, LAVH, and Laparoscopic Hysterectomy. Vaginal hysterectomy requires only a vaginal incision through which the uterus is removed. The vaginal incision is closed with stitches.
A variation of the vaginal approach is called laparoscopic-assisted vaginal hysterectomy (LAVH). It uses several small abdominal incisions through which the surgeon severs the attachments to the uterus and, if needed, ovaries. In LAVH, the uterus (and ovaries) are then removed through the vaginal incision, as in the standard vaginal approach. In laparoscopic hysterectomy, they are removed in small pieces through the abdomen.
Recovery times for vaginal hysterectomy and LAVH are shorter than those for abdominal hysterectomy. However, hospital stays may be longer, and costs are greater with LAVH than with standard vaginal hysterectomy. Some doctors question whether LAVH adds any significant benefits compared to the standard vaginal procedure.
Robotic Hysterectomy. Robotic hysterectomy is like laparoscopic hysterectomy, but a special machine is used. This approach is most often used when a patient has cancer or is very overweight and vaginal surgery is not safe.
Complications
Minor complications after hysterectomy are very common. About half of women develop minor and treatable urinary tract infections. There is usually mild pain and light vaginal bleeding post operation. More serious complications are uncommon but can include infection and blood clots.
Postoperative Care
The patient should ask a family member or friend to help out for the first few days at home. The following are some of the precautions and tips for postoperative care:
- For 1 - 2 days after surgery, the patient is given medications to prevent nausea and painkillers to relieve pain at the incision site.
- As soon as the doctor recommends it, usually within a day of the operation, the patient should get up and walk in order to help prevent pneumonia, reduce the risk of blood-clot formation, and speed recovery.
- Walking and slow, deep breathing exercises may help to relieve gas pains, which can cause major distress for the first few days.
- Coughing can cause pain, which may be reduced by holding a pillow over a surgical abdominal wound or by crossing the legs after vaginal surgery.
- Patients are advised not to lift heavy objects, not to douche or take baths, and not to climb stairs or drive for several weeks.
- For the first few days after surgery, many women weep frequently and unexpectedly. These mood swings may be due to depression from the loss of reproductive capabilities and from abrupt changes in hormones, particularly if the ovaries have been removed.
Patients who have had abdominal hysterectomies should discuss with their doctors when exercise programs more intense than walking can be started. The abdominal muscles are important for supporting the upper body, and recovering strength may take a long time. Even after the wound has healed, the patient may have an on-going feeling of overall weakness, for some time. Some women do not feel completely well for as long as a year while others may recover in only a few weeks.
If a woman has had her cervix removed, she no longer needs annual Pap smears. However, women who have had any type of hysterectomy should continue to receive routine pelvic and breast exams, and mammograms.
Menopausal Symptoms and Premature Menopause after Hysterectomy
The ovaries are the main source of production of estrogen. In premenopausal woman, the removal of ovaries causes premature menopause. After hysterectomy with bilateral oopherectomy, women may have hot flashes and other symptoms of menopause, including vaginal dryness, insomnia, and weight gain.
Women who have surgical removal of both ovaries, and who do not receive hormone replacement therapy, tend to have more severe hot flashes than women who enter menopause naturally. If hormone replacement therapy (HRT) is recommended after hysterectomy and ovary removal, it is given as estrogen-only replacement therapy (ERT). (Women without ovaries do not need to take combination estrogen-progesterone HRT.)
In premenopausal women who have had their ovaries retained, the ovaries will usually continue to function and secrete hormones even after the uterus is removed, but the lifespan of the ovaries is reduced by an average of 3 - 5 years. In rare cases, complete ovarian failure occurs right after hysterectomy, presumably because the surgery has permanently cut off the ovaries' blood supply.
The most important complications occur in women who have had their ovaries removed. This causes estrogen loss, which places women at risk for osteoporosis (loss of bone density) and a possible increase in risks for heart disease and stroke. Several drugs are available that can help protect both bones and heart.
Sexuality after Hysterectomy
Sexual intercourse may resume 4 - 6 weeks following surgery. The effect of hysterectomy on sexuality varies among women. Some women notice a change in their orgasmic response because they no longer experience uterine contractions. Other women report increased sexual drive and pleasure because they are free from the problems that prompted hysterectomy.
Patients who have both ovaries removed may be at higher risk for loss of sexuality and experience sexual problems such as vaginal dryness. A vaginal gel or lubricant can help reduce vaginal dryness.
Resources
- www.asrm.org -- American Society for Reproductive Medicine
- www.acog.org -- American College of Obstetricians and Gynecologists
- www.sirweb.org -- Society of Interventional Radiology
- www.nuff.org -- National Uterine Fibroids Foundation
- www.rsna.org -- Radiological Society of North America
- www.radiologyinfo.org -- Radiology info from the American College of Radiology and the Radiological Society of North America
- www.womenshealth.gov -- National Women's Health Information Center
References
American College of Obstetricians and Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008 Aug;112(2 Pt 1):387-400.
Bradley LD. Uterine fibroid embolization: a viable alternative to hysterectomy. Am J Obstet Gynecol. 2009 Aug;201(2):127-35.
Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion; Centers for Disease Control and Prevention (CDC), Farr S, Folger SG, Paulen M, et al. U S. Medical Eligibility Criteria for Contraceptive Use, 2010: adapted from the World Health Organization Medical Eligibility Criteria for Contraceptive Use, 4th edition. MMWR Recomm Rep. 2010 Jun 18;59(RR-4):1-86.
Edwards RD, Moss JG, Lumsden MA, Wu O, Murray LS, Twaddle S, et al. Uterine-artery embolization versus surgery for symptomatic uterine fibroids. N Engl J Med. 2007 Jan 25;356(4):360-70.
Evans P, Brunsell S. Uterine fibroid tumors: diagnosis and treatment. Am Fam Physician. 2007 May 15;75(10):1503-8.
Goodwin SC, Spies JB. Uterine fibroid embolization. N Engl J Med. 2009 Aug 13;361(7):690-7.
Griffiths A, D'Angelo A, Amso N. Surgical treatment of fibroids for subfertility. Cochrane Database Syst Rev. 2006 Jul 19;3:CD003857.
Homer H, Saridogan E. Uterine artery embolization for fibroids is associated with an increased risk of miscarriage. Fertil Steril. 2010 Jun;94(1):324-30. Epub 2009 Apr 9.
Jacoby VL, Grady D, Sawaya GF. Oophorectomy as a risk factor for coronary heart disease. Am J Obstet Gynecol. 2009 Feb;200(2):140.e1-9. Epub 2008 Nov 18.
Kaunitz AM. Progestin-releasing intrauterine systems and leiomyoma. Contraception. 2007 Jun;75(6 Suppl):S130-3. Epub 2007 Mar 9.
Kaunitz AM, Meredith S, Inki P, Kubba A, Sanchez-Ramos L. Levonorgestrel-releasing intrauterine system and endometrial ablation in heavy menstrual bleeding: a systematic review and meta-analysis. Obstet Gynecol. 2009 May;113(5):1104-16.
Lethaby A, Hickey M, Garry R, Penninx J. Endometrial resection / ablation techniques for heavy menstrual bleeding. Cochrane Database Syst Rev. 2009 Oct 7;(4):CD001501.
Moss J, Cooper K, Khaund A, Murray L, Murray G, Wu O, et al. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG. 2011 Jul;118(8):936-944. doi: 10.1111/j.1471-0528.2011.02952.x. Epub 2011 Apr 12.
Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD003677.
[No authors listed] ACOG Practice Bulletin No. 110: noncontraceptive uses of hormonal contraceptives. Obstet Gynecol. 2010 Jan;115(1):206-18.
Olive DL, Lindheim SR, Pritts EA. Conservative surgical management of uterine myomas. Obstet Gynecol Clin North Am. 2006 Mar;33(1):115-24.
Parker WH, Broder MS, Chang E, Feskanich D, Farquhar C, Liu Z, et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses' health study. Obstet Gynecol. 2009 May;113(5):1027-37.
Smart OC, Hindley JT, Regan L, Gedroyc WG. Gonadotrophin-releasing hormone and magnetic-resonance-guided ultrasound surgery for uterine leiomyomata. Obstet Gynecol. 2006 Jul;108(1):49-54.
Stokes LS, Wallace MJ, Godwin RB, Kundu S, Cardella JF;Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomas. J Vasc Interv Radiol. 2010 Aug;21(8):1153-63. Epub 2010 Jun 16.
Stout MJ, Odibo AO, Graseck AS, Macones GA, Crane JP, Cahill AG. Leiomyomas at routine second-trimester ultrasound examination and adverse obstetric outcomes. Obstet Gynecol. 2010 Nov;116(5):1056-63.
Van Voorhis B. A 41-year-old woman with menorrhagia, anemia, and fibroids: review of treatment of uterine fibroids. JAMA. 2009 Jan 7;301(1):82-93. Epub 2008 Dec 2.
van der Kooij SM, Bipat S, Hehenkamp WJ, Ankum WM, Reekers JA. Uterine artery embolization versus surgery in the treatment of symptomatic fibroids: a systematic review and metaanalysis. Am J Obstet Gynecol. 2011 Oct;205(4):317.e1-18. Epub 2011 Mar 16.
Volkers NA, Hehenkamp WJ, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids: 2 years' outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2007 Jun;196(6):519.e1-11.
|
Review Date:
9/10/2012 Reviewed By: Reviewed by Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |





