Gout
Highlights
- Gout is a painful inflammatory arthritis condition caused by deposits of uric acid crystals in the joints and soft tissues. The painful attacks often begin at night and may last for a week.
- An estimated 6.1 million adults in the U.S. have gout. The incidence and prevalence of gout is growing in the U.S. This is most likely due to obesity, an aging population, and the use of diuretics.
- If gout is diagnosed properly, it is relatively easy for doctors and patients to treat the condition. Adherence to medication and lifestyle recommendations is key to managing chronic gout. However, patient compliance can pose a challenge since the condition is asymptomatic between attacks.
Guidelines
- The American College of Rheumatology is currently developing new guidelines for the management of gout.
- The European League Against Rheumatism (EULAR) and the British Society for Rheumatology have published guidelines for the evaluation and management of gout.
Medication
- In September 2010, the FDA approved Krystexxa (pegloticase) IV injections for the treatment of gout. Injections are given every two or four weeks, but are reserved for patients with severe chronic gout who have not been helped by first line treatments, such as allopurinol. Krystexxa is an enzyme, or biologic, that targets uric acid directly by transforming it into a different molecule.
- The FDA only recently approved colchicine (Colcyrs) for the treatment of acute gout, but doctors have been prescribing this medication (as well as NSAIDs) for decades.
Research
- The Nurses' Health Study, a 22 year follow-up study, showed that consumption of fructose, sugar-sweetened soda, and orange juice was associated with gout in women. This same association has been shown in studies of men. However, the incidence of gout among women is small compared to men, and several other factors may contribute to gout in women.
- How low uric acid levels should be and the duration of uric acid lowering treatment is unclear. Researchers are looking at possible associations between low uric acid levels and other conditions. Further study is needed.
- Interleukin-1 antagonists are also being studied as agents for acute gout attacks, but more research is necessary.
Introduction
Gout is a painful and common type of arthritis. About 1 in 100 people develop gout. The condition is usually associated with a long-lasting, abnormally high amount of uric acid in the blood, called chronic hyperuricemia.
The rate of gout has increased in recent decades, not only in America but also in other developed countries. The increase is most likely due to dietary and lifestyle changes, greater use of medications, such as diuretics, that boost uric acid levels, and aging populations. Gout is very uncommon in developing countries.
How Gout and Hyperuricemia Occur
Metabolism of Purines. The process leading to hyperuricemia and gout begins with the metabolism of purines, nitrogen-containing compounds that are important for energy. Purines can be divided into two types:
- Endogenous purines are manufactured within human cells.
- Exogenous purines are obtained from foods.
The process of breaking down purines results in the formation of uric acid in the body. Most mammals have an enzyme called uricase, which breaks down uric acid so it can be easily removed from the body. Because humans lack uricase, uric acid is not as easily removed, and can build up in body tissues.
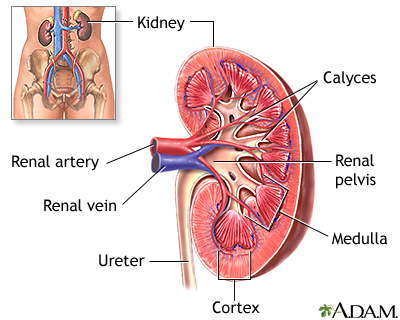
Uric Acid and Hyperuricemia. Purines in the liver produce uric acid. The uric acid enters the bloodstream, and most of it eventually goes through the kidneys and is excreted in the urine. The remaining uric acid travels through the intestines, where bacteria help break it down.
Normally these actions keep the level of uric acid in the blood plasma (the liquid part of the blood) at a healthy level, which is below 6.8 mg/dL. But under certain circumstances, the body produces too much uric acid or removes too little. In either case, concentrations of uric acid increase in the blood. This condition is known as hyperuricemia.
If concentrations of uric acid in the blood reach 7 mg/dL and above, needlelike crystals of a salt called monosodium urate (MSU) are likely to begin to form. The higher the levels of uric acid in the blood, the higher the risk for crystal formation. As crystals build up in the joints, they trigger inflammation and pain, the characteristic symptoms of gout.
Symptoms
The specific symptoms of gout depend on the stage of the disease. Gout is often divided into four stages:
- Asymptomatic hyperuricemia
- Acute gouty arthritis
- Intercritical gout
- Chronic tophaceous gout
Asymptomatic Hyperuricemia
Asymptomatic means there are no symptoms. Asymptomatic hyperuricemia is considered the first stage of gout. Urate levels slowly increase in the body. This stage may last for 30 years or more.
Note: Hyperuricemia does not inevitably lead to gout. In fact, less than 20% of cases turn out to be full-blown arthritic gout disease.
Symptoms of Acute Gouty Arthritis
Acute gouty arthritis occurs when the first symptoms of gout appear. Sometimes the first signs of gout are brief twinges of pain (petit attacks) in an affected joint. These attacks can precede the actual full-blown condition by several years.
Symptoms of acute gouty arthritis include:
- Severe pain at and around the joint
- May feel like "crushing" or a dislocated bone
- Physical activity and even the weight of bed sheets may be unbearable
- Usually takes 8 - 12 hours to develop
- Occurs late at night or early in the morning and may wake you up
- Swelling that may extend beyond the joint
- Warmth over the joint
- Red, shiny, tense skin over the affected area, which may peel after a few days
- Chills and mild fever, loss of appetite, and feelings of ill health
Most often symptoms start in one joint.
Monoarticular Gout. Gout that occurs in one joint is called monoarticular gout. About 60% of all first-time monoarticular gout attacks in middle-aged adults occur in the big toe. This occurrence is known as podagra. Symptoms can also occur in other locations, such as the ankle or knee.
Polyarticular Gout. If more than one joint is affected, the condition is known as polyarticular gout. Multiple joints are affected in only 10 - 20% of first attacks. Older people are more likely to have polyarticular gout. The most frequently affected joints are the foot, ankle, knee, wrist, elbow, and hand. The pain usually occurs in joints on one side of the body and it is usually, although not always, in the lower legs and the feet. People with polyarticular gout are more likely to have a slower onset of pain and a longer delay between attacks. People with polyarticular gout are also more likely to experience low-grade fever, loss of appetite, and a general feeling of poor health.
An untreated attack will typically peak 24 - 48 hours after the first appearance of symptoms, and go away after 5 - 7 days. However, some attacks last only hours, while others persist as long as several weeks. Though symptoms can subside, the crystals are still present, and future attacks are likely to occur.
Intercritical Gout
Intercritical gout is the term used to describe the periods between attacks. The first attack is usually followed by a complete remission of symptoms, but, if left untreated, gout nearly always returns. Over two-thirds of patients will have at least one further attack within 2 years of the first attack. By 10 years, over 90% of the patients are likely to have repeat attacks.
Symptoms of Chronic Tophaceous Gout
Chronic Tophaceous Gout and Tophi. After several years, persistent gout can develop into a condition called chronic tophaceous gout. This long-term condition often produces tophi, which are solid deposits of MSU crystals that form in the joints, cartilage, bones, and elsewhere in the body. In some cases, tophi break through the skin and appear as white or yellowish-white, chalky nodules that have been described as looking like crab eyes.
Without treatment, tophi may develop about 10 years after the initial onset of gout, although the occurrence can range from 3 - 42 years. Tophi are more likely to appear early in the course of the disease in older people. In the elderly population, women appear to be at higher risk for tophi than men. Certain people, such as those who are receiving cyclosporine after a transplant, have a high risk of developing tophi.
Development of Chronic Pain. When gout remains untreated, the intercritical periods typically become shorter and shorter, and the attacks, although sometimes less intense, can last longer. Over the long term (about 10 - 20 years) gout becomes a chronic disorder characterized by constant low-grade pain and mild or acute inflammation. Gout may eventually affect several joints, including those that may have been free of symptoms at the first appearance of the disorder. In rare cases, the shoulders, hips, or spine are affected.
Location of Tophi. Tophi generally form in the following locations:
- Curved ridge along the edge of the outer ear
- Forearms
- Elbow or knee
- Hands or feet -- older patients, particularly women, are more likely to have gout in the small joints of the fingers.
- Around the heart and spine (rare)
Tophi are generally painless. However, they can cause pain and stiffness in the affected joint. Eventually, they can also erode cartilage and bone, ultimately destroying the joint. Large tophi under the skin of the hands and feet can give rise to extreme deformities.
Complications
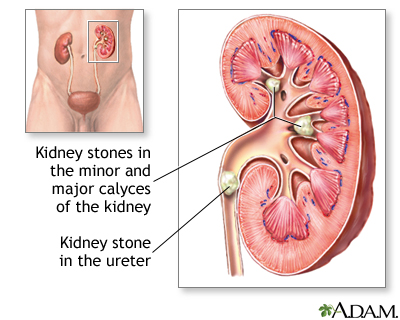
Uric Acid Nephrolithiasis (Kidney Stones). Persons who have kidney stones that formed from uric acid are more likely to have higher levels of uric acid in their blood than in their urine. This suggests that gout is responsible for this type of kidney stones. Uric acid stones and other forms of kidney stones are present in 10 - 25% of patients with primary gout, a rate of more than 1,000 times that of the general population. In gout caused by other conditions (called secondary gout), the reported rate reaches 42%.
Not all of the kidney stones in patients with gout are made of uric acid. Some are made from calcium oxalate, calcium phosphate, or substances combined with uric acid. Uric acid stones can also form when you do not have gout or hyperuricemia.
Chronic Uric Acid Interstitial Nephropathy. Chronic uric acid interstitial nephropathy occurs when crystals slowly form in the structures and tubes that carry fluid from the kidney. It is reversible and not likely to injure the kidneys.
Kidney Failure. Sudden overproduction of uric acid can occasionally block the kidneys and cause them to fail. This occurrence is very uncommon but can develop after any of the following:
- Chemotherapy for leukemia or lymphoma, particularly acute forms of the disease
- Other cancers, such as breast cancer and lung cancer
- Epileptic seizures
- Pregnancy related preeclampsia or eclampsia
- Use of medications to prevent kidney transplant rejection, such as cyclosporine
Causes and Risk Factors
Gout is classified as either primary or secondary, depending on what causes the high levels of uric acid in the blood (hyperuricemia).
More than 99% of primary gout cases are referred to as idiopathic, meaning that the cause of the hyperuricemia cannot be determined. Primary gout is most likely the result of a combination of genetic, hormonal, and dietary factors. Secondary gout is caused by drug therapy or by medical conditions other than a metabolic disorder.
The following factors increase the risk for gout:
- Advancing age
- Male gender
- Family history of the condition; genetic predisposition
- Obesity
- Use of certain drugs, including diuretics ("water pills"), low-dose aspirin, cyclosporine, or levodopa
- Binge drinking
- Lead toxicity
- Organ transplants
- Thyroid problems
- Other serious illness
People with gout are at an increased risk of having metabolic syndrome. Metabolic syndrome is a collection of problems, such as abdominal obesity, high blood pressure, and low "good" cholesterol. This syndrome increases a person's risk of heart disease and stroke. Therefore, lifestyle changes are an important aspect of the prevention of gout and improvement of overall health.
Each risk factor is discussed in more detail below.
Age
Middle-Aged Adults. Gout usually occurs in middle-aged men, peaking in the mid-40s. It is most often associated in this age group with obesity, high blood pressure, unhealthy cholesterol levels, and heavy alcohol use.
Elderly. Gout can also develop in older people, when it occurs equally in men and women. In this group, gout is most often associated with kidney problems and the use of diuretics. It is less often associated with alcohol use.
Children. Except for rare inherited genetic disorders that cause hyperuricemia, gout in children is rare.
Gender
Men. Men are significantly at higher risk for gout. In males, uric acid levels rise substantially at puberty. In about 5 - 8% of American men, levels exceed 7 mg/dL (indicating hyperuricemia). However, gout typically strikes after 20 - 40 years of persistent hyperuricemia, so men who develop it usually experience their first attack between the ages of 30 and 50.
Women. Before menopause, women have a significantly lower risk for gout than men, possibly because of the actions of estrogen. This female hormone appears to facilitate uric acid excretion by the kidneys. (Only about 15% of female gout cases occur before menopause.) After menopause the risk increases in women. At age 60 the incidence is equal in men and women, and after 80, gout occurs more often in women.
Family History/Genetics
A family history of gout is present in close to 20% of patients with this condition. Several genes have been associated with the body's uric acid metabolism and gout. Some people with a family history of gout have a defective protein (enzyme) that interferes with the way the body breaks down purines.
Obesity
Researchers report a clear link between body weight and uric acid levels. In one Japanese study, overweight people had two to more than three times the rate of hyperuricemia as those who maintained a healthy weight. Children who are obese may have a higher risk for gout in adulthood.
Medications
Thiazide diuretics are "water pills" used to control hypertension. The drugs are strongly linked to the development of gout. A large percentage of patients who develop gout at an older age report the use of diuretics.
Several other medications can increase uric acid levels and raise your risk for gout. These include:
- Aspirin -- low doses of aspirin reduce uric acid excretion and increase the chance for hyperuricemia. This may be a problem for older people who take baby aspirin (81 mg) to protect against heart disease.
- Niacin (used to treat cholesterol problems)
- Pyrazinamide (used to treat tuberculosis)
Alcohol
Drinking excessive amounts of alcohol can raise your risk of gout. Beer is the kind of alcohol most strongly linked with gout, followed by spirits. Moderate wine consumption does not appear to increase the risk of developing gout.
Alcohol use is highly associated with gout in younger adults. Binge drinking particularly increases uric acid levels. Alcohol appears to play less of a role among elderly patients, especially among women with gout.
Alcohol increases uric acid levels in the following three ways:
- Providing an additional dietary source of purines (the compounds from which uric acid is formed)
- Intensifying the body's production of uric acid
- Interfering with the kidneys' ability to excrete uric acid
Lead Exposure
Chronic occupational exposure to lead is associated with build-up of uric acid and a high incidence of gout.
Organ Transplants
Kidney transplantation poses a high risk for renal insufficiency and gout. In addition, other transplantation procedures, such as heart and liver, increase the risk of gout. The procedure itself poses a risk of gout, as does the medication (cyclosporine) used to prevent rejection of the transplanted organ. Cyclosporine also interacts with indomethacin, a common gout treatment.
Other Illnesses
Treatment of several other conditions can cause significant elevations of uric acid in the blood, and therefore a gout attack. These conditions include:
- Leukemia
- Lymphoma
- Psoriasis
Triggers
Triggers are events or conditions that can set off a gout attack. Certain risk factors, including a purine-rich diet, are also considered a trigger. Triggers include:
- Joint injury
- Overindulging in alcohol or purine-rich foods
- Dehydration
- Severe illness or infection
- Sudden weight loss, "crash diets"
- Surgery
- Radiation therapy
- Using certain drugs
Hot and humid weather may also be strongly associated with recurrent gout attacks. Such weather can cause sweating and, ultimately, dehydration, which has long been recognized as a potential trigger for gout attacks.
Drinking more water and fluids when it's warm outside could help persons with gout prevent future attacks.
Diagnosis
The first step in diagnosing the disease is to determine which joints are affected. A physical examination and medical history can help confirm or rule out gout. For example, gout is more likely if arthritis first appears in the big toe.
The speed of the onset of pain and swelling is also important. Symptoms that take days or weeks (rather than hours) to develop probably indicate a disorder other than gout.
Abnormal enlargements in joints that had been affected by previous injury or osteoarthritis are possible signs of gout. This is particularly significant in older women who take diuretics ("water pills").
Studies have shown that family physicians are able to diagnose gout reasonably well using simple diagnostic information including specific symptoms, history, and lifestyle factors. However, aspiration of fluid from the inflamed joint is the most definitive diagnostic test.
Blood Test for Uric Acid Levels
A blood test is usually done to measure uric acid levels and detect hyperuricemia. A low level of uric acid in the blood makes a diagnosis of gout much less probable, and a very high level increases the likelihood of gout, especially if patient has symptoms of gout. Nevertheless, uric acid levels in the blood during an attack of gout can be within or below the normal range, and the presence of hyperuricemia does not necessarily mean someone has gout. However, most doctors feel that closer monitoring of blood uric acid levels in people with gout may help reduce gout flares. Other blood tests may also help distinguish gout from other arthritic conditions. A patient with high uric acid levels and acute onset of pain in a characteristic joint has an 82% chance of having gout.
Examination of Synovial Fluid
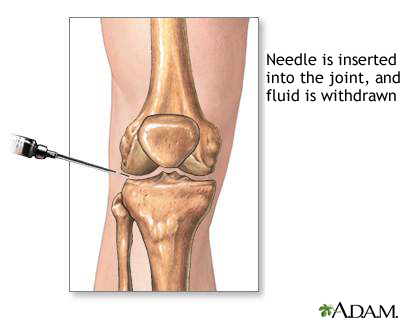
Synovial fluid examination is the most accurate method for diagnosing gout. The synovial fluid is the lubricating liquid that fills the synovium (the membrane that surrounds a joint and creates a protective sac). The fluid cushions joints and supplies nutrients and oxygen to the cartilage surface that coats the bones. This exam also helps detect gout between attacks.
A procedure called arthrocentesis is performed. The health care provider uses a needle attached to a syringe to draw out fluid from the affected joint. This is called aspiration. Local anesthesia is not used because it can reduce the effectiveness of the procedure. However, the procedure is usually only mildly uncomfortable. Afterwards, there can be some minor discomfort in the area where the needle was inserted, but it usually goes away quickly.
The fluid sample is sent to a laboratory for analysis. Testing can reveal the presence of monosodium urate (MSU) crystals, which will nearly always confirm a diagnosis of gout. The laboratory can also test the sample for infection.
The procedure itself can cause infection, though this occurs in less than 0.1% of patients. Aspiration sometimes eases the patient's symptoms by reducing swelling and pressure on the tissue surrounding the joint.
Urine Tests
It is sometimes helpful to gauge the amount of uric acid found in a patient's urine, particularly if the patient is young and has pronounced hyperuricemia that might be related to a metabolic disorder. If uric acid in the urine exceeds a particular value, further tests for an enzyme defect or other identifiable cause of gout should be performed. Greater-than-normal amounts of uric acid in the urine also mean that the patient is more likely to develop uric acid kidney stones.
Typically, a 24-hour urine test is performed. The patient discards the first urination sample on the day of the test. Afterward all urine passed over the next 24 hours is collected into a special container, including the first urination on the morning of day two. The container is delivered to the patient's health care provider or sent directly to the laboratory.
The urine is collected between attacks, after the patient has been placed on a purine-reduced diet. The patient is also asked to temporarily stop using alcohol and any medications that can interfere with the test. The patient should not change any of his or her usual eating or drinking patterns when performing this test.
Imaging Tests
X-Rays. For the most part, x-rays do not reveal any problems during the early stages of gout. Their usefulness lies in assessing the progress of the disorder in its chronic phase and identifying other health problems with symptoms similar to gout. Tophi can be seen on x-rays before they become apparent on physical examination.
Advanced Imaging Techniques. Advanced imaging techniques being investigated for identifying tophi include computed tomography (CT), magnetic resonance imaging (MRI), and Doppler ultrasonography.
Ruling out Other Disorders
As part of the diagnosis, other disorders that produce gout-like symptoms or cause hyperuricemia should be ruled out. In general, it is easy to distinguish acute gout that occurs in one joint from other arthritic conditions. The two disorders that may confuse this diagnosis are pseudogout and septic arthritis. Pseudogout is a condition most likely to be confused with gout.
Chronic gout can often resemble rheumatoid arthritis. Several other conditions may at some point in their course resemble gout.
Pseudogout (Calcic Gout)
Pseudogout (also called calcic gout and calcium pyrophosphate dihydrate deposition disease) is a common inflammatory arthritis among older adults. Very similar to gout, pseudogout is caused by deposits of calcium pyrophosphate dihydrate crystals in and around the joints.
Although symptoms of pseudogout resemble gout in some ways, there are differences:
- The first attack typically strikes the knee. Other joints commonly affected are the shoulders, wrists, and ankles. At least two-thirds of cases affect more than one joint during a first attack. Pseudogout may involve any joint, although the small joints in the fingers or toes are not commonly affected.
- The symptoms of pseudogout also appear more slowly than those of gout, taking days rather than hours to develop.
- Pseudogout is more likely to first develop in elderly people, particularly those with osteoarthritis. (It affects 10 - 15% of people over 65.)
Pseudogout is more likely to occur in the autumn while gout attacks are most common in the spring.
Who Gets Pseudogout?
Conditions that are associated with a higher risk for pseudogout in elderly patients include underlying acute medical conditions, trauma, or surgery. Medical conditions associated with pseudogout include hypothyroidism, diabetes, gout, and osteoarthritis. Liver transplantation also may increase the risk.
How Is Pseudogout Treated?
There is no cure for pseudogout. It is a progressive disorder that can eventually destroy joints. Treatments for pseudogout are similar to those for gout and are aimed at relieving the pain and inflammation and reducing the frequency of attacks.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are effective for treating inflammation and pain from pseudogout.
- For acute attacks in large joints, fluid aspiration alone or with corticosteroids may help.
- Colchicine may be used for acute attacks.
- Magnesium carbonate may help dissolve crystals, but existing hard deposits may remain.
- Surgery may be required for joint replacement.
Other Disorders
Rheumatoid Arthritis. Rheumatoid arthritis can distort the joints of the finger and cause inflammation and pain that may mimic gout. In older people, it is particularly difficult to distinguish chronic gout from rheumatoid arthritis. A proper diagnosis can be made with a detailed medical history, laboratory tests, and identification of MSU crystals.
Osteoarthritis. Gout can coincide and be confused with osteoarthritis in older people, particularly when it occurs in arthritic finger joints in women. In general, gout should be suspected if the joints in the fingertips are unusually enlarged.
Infections. Joint infections can have features that resemble gout. A correct diagnosis is critical for appropriate treatment. For example, some cases of gout have been confused with infection after joint replacement. On the other hand, joint infection not associated with surgery might indicate sepsis, which is a widespread and potentially life-threatening bacterial infection that can cause inflamed joints, chills, and a spiking fever. The severity of the fever and a high white blood cell count in the joint fluid helps diagnose a septic infection, while urate crystals in the joint are a good indicator of gout.
Charcot Foot. People with diabetes who also have problems in the nerves in the feet (diabetic peripheral neuropathy) may develop Charcot foot or Charcot joint (medically referred to as neuropathic arthropathy). Early changes may resemble gout, with the foot becoming swollen, red, and warm, although it involves other parts of the foot besides the large toe. Recognition and treatment of this condition is very important. A seriously affected foot can become deformed. The bones may crack, splinter, and erode, and the joints may shift, change shape, and become unstable.
Bunions. A bunion is a foot deformity that usually occurs at the head of the first of five long bones (the metatarsal bones) that extend from the arch and connect to the toes, and may be confused with gout. The first metatarsal bone is the one that attaches to the big toe. A bunion begins to form when the big toe is forced in toward the rest of the toes, causing the head of the first metatarsal bone to jut out and rub against the side of the shoe. The underlying tissue becomes inflamed, and a painful bump forms. As this bony growth develops, the bunion is formed as the big toe is forced to grow at an increasing angle towards the rest of the toes.
Some Diseases with Symptoms Similar to Gout | |
Disease | Specific Subtypes |
Osteoarthritis | |
Infectious Arthritis | Lyme disease, bacterial arthritis, tuberculous and fungal arthritis, viral arthritis, osteomyelitis |
Postinfectious or Reactive Arthritis | Reiter syndrome (a disorder characterized by arthritis and inflammation in the eye and urinary tract), rheumatic fever, inflammatory bowel disease |
Pseudogout | |
Rheumatic Autoimmune Diseases | Rheumatoid arthritis, systemic vasculitis, systemic lupus erythematosus, scleroderma, Still's disease (also called juvenile rheumatoid arthritis) |
Fracture or Trauma Fibromyalgia | |
Other Diseases | Chronic fatigue syndrome, hepatitis C, familial Mediterranean fever, cancers, AIDS, leukemia, bunions, Whipple's disease, dermatomyositis, Behcet's disease, Henoch-Schonlein purpura, Kawasaki's disease, erythema nodosum, erythema multiforme, pyoderma gangrenosum, psoriatic arthritis |
Treatment: Acute Gout Attack
Acute attacks of gout and long-term treatment of gout and hyperuricemia require different approaches. Treatment usually involves medication. After the first attack, some health care providers advise their patients to keep a supply of medications on hand so that self-medication can begin at the first sign of symptoms of a second acute attack. There are also specific treatments for conditions associated with gout, including uric acid nephropathy and uric acid nephrolithiasis.
Supportive measures include applying ice and resting the affected joint.
Many patients do not require medications. During the period between gout attacks, patients are advised to avoid foods high in purines and to maintain a healthy weight. Patients should also avoid excessive alcohol consumption and reduce any stress.
Drug treatments for acute attacks of gout are aimed at relieving pain and reducing inflammation. They should be started as early as possible.
Medications used in the treatment of gout include:
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- Colchicine
- Corticosteroids
- Adrenocorticotropic Hormone
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Powerful forms of nonsteroidal anti-inflammatory drugs (NSAIDs) are the drugs of choice for an acute attack in younger, healthy patients with no serious health problems, particularly problems that affect the kidneys, liver, or heart.
Many NSAIDs are available. Over-the-counter NSAIDs include:
- Low-dose Ibuprofen (Motrin IB, Advil, Nuprin)
- Naproxen (Aleve)
- Ketoprofen (Actron, Orudis KT)
Prescription NSAIDs include:
- Ibuprofen (Motrin)
- Naproxen (Naprosyn, Anaprox)
- Flurbiprofen (Ansaid)
- Diclofenac (Voltaren)
- Tolmetin (Tolectin)
- Ketoprofen (Orudis, Oruvail)
- Dexibuprofen (Seractil)
- Indomethacin (Indocin)
Indomethacin (Indocin) is typically the first choice of treatment for patients who have no medical conditions that would interfere with its use. Usually 2 - 7 days of high-dose indomethacin is enough to treat a gout attack. The first dose of indomethacin usually begins to act against the pain and inflammation within 24 hours and often much sooner.
Ibuprofen, naproxen, sulindac, or other NSAIDs are good alternatives, particularly for elderly patients who might experience confusion or bizarre sensations with indomethacin. (Aspirin is an NSAID, but it is associated with a higher risk for gout and should be avoided.)
Regular use of even over-the-counter NSAIDs can cause certain health problems, such as:
- Ulcers and gastrointestinal bleeding
- Increased blood pressure -- people with hypertension, severe vascular disease, kidney, or liver problems and those taking diuretics must be closely monitored if they need to take NSAIDs.
- Delayed emptying of the stomach, which could interfere with the actions of other drugs. The elderly are at special risk.
- Dizziness
- Tinnitus (ringing in the ear)
- Headache
- Skin rash
- Depression
- Confusion or bizarre sensation (in some higher-potency NSAIDs, notably indomethacin)
- Kidney damage
NSAIDs can cause kidney problems, especially in the elderly and those with kidney disease. When caught early enough, these problems generally resolve if the drugs are stopped. Any sudden weight gain or swelling should be reported to a physician. Anyone with kidney disease should avoid these drugs.
Patients with diabetes who take hypoglycemics by mouth may need to adjust their medication dosage if they also take NSAIDs, because of possible harmful interactions between these classes of drugs.
NSAID-Induced Ulcers and Gastrointestinal Bleeding
Long-term use of NSAIDs is a common cause of ulcers. NSAID-related bleeding and stomach problems may be responsible for over 100,000 hospital admissions and over 15,000 deaths each year. Because there are usually no gastrointestinal symptoms from NSAIDs until bleeding begins, health care providers cannot predict which patients taking these drugs will develop bleeding.
Those at high risk for NSAID-related bleeding include the elderly, anyone with a history of an ulcer or gastrointestinal bleeding, patients with serious heart conditions, those who drink too much alcohol, and persons on certain medications, such anticoagulants (blood thinners), corticosteroids, or bisphosphonates (drugs used for osteoporosis).
Preventing NSAID-Related Ulcers. Switching to alternative pain relievers is the first step in preventing or healing ulcers caused by NSAIDs. If people cannot change drugs, they should use the lowest NSAID dose possible.
In addition, medications are available that may help prevent ulcers in people who need to take NSAIDs. Proton-pump inhibitors (PPIs) are the first drug of choice for preventing ulcers in high-risk individuals. They have been shown to reduce NSAID-ulcer rates by as much as 80% compared with no treatment. Types of these drugs include omeprazole (Prilosec), esomeprazole (Nexium), lansoprazole (Prevacid), rabeprazole (AcipHex ), and pantoprazole (Protonix). Prevacid is the first proton-pump inhibitor specifically approved for protecting against ulcers in chronic NSAID users.
Arthrotec is a combination of an ulcer-protective drug called misoprostol and the NSAID diclofenac. It too may reduce the risk for gastrointestinal bleeding. The drug can cause miscarriages, however, and should not be taken by women who are pregnant or plan to become pregnant.
Corticosteroids
Corticosteroids may be used in patients who cannot tolerate NSAIDs and they may be particularly beneficial for elderly patients. Injections into an affected joint provide effective relief for many patients, but this is not useful for patients who have multiple affected joints. Steroids taken by mouth may be used for patients who cannot take NSAIDs or colchicine and who have gout in more than one joint.
Glucocorticoids or corticotropin may be given when NSAIDs are not well tolerated, or contraindicated. Corticosteroids include triamcinolone and prednisone.
Colchicine
Colchicine is a derivative of the autumn crocus (also called the meadow saffron). It has been used against gout attacks for centuries, though only recently approved by the FDA (Colcyrs). It is highly effective in relieving a gout attack. It is not typically the first drug of choice because it may cause unpleasant, and sometimes serious side effects. It is recommended as a second line therapy when NSAIDS and corticosteroids either can't be tolerated or are ineffective. Side effects may include stomach upset, vomiting, and diarrhea. New recommendations call for lower, incremental dosing throughout the gout attack up to a maximum total dose (or until stomach upset occurs).
Colchicine may be given orally to a healthy adult within 48 hours of an attack. It should not be used by elderly patients or those with kidney, liver, or bone marrow disorders. It can also affect fertility and should not be used during pregnancy. It comes in low dose tablet form. Certain patients require close monitoring while taking colchicine.
The antibiotic erythromycin, or H2 blockers such as famotidine (Pepcid AC), cimetidine (Tagamet), or ranitidine (Zantac) may intensify the gastrointestinal side effects of colchicine.
Warning Note: Overdose of colchicine can be dangerous, and there have even been reports of death. The drug may also suppress blood cell production and cause nerve and muscular injury in certain people. Close monitoring for toxicity is essential.
Treatment: Preventing Attacks
Between Attacks
After an acute attack some patients remain at high risk for another attack for several weeks during the intercritical period. Such patients include those with kidney insufficiency or those with congestive heart failure who are on diuretics. Low doses of colchicine or NSAIDs may be used to during this period for prevention of another attack. They should be taken in low doses for 1 - 2 months after an attack, or for longer periods in patients who have experienced frequent attacks.
Medicines to Lower Uric Acid Levels
Medicines which help lower uric acid levels in the blood and thus prevent gout attacks and other complications can be prescribed. The decision whether to use these medicines and at what point is not entirely clear. Some health care providers do not prescribe them if hyperuricemia is mild, or until a patient has had two gout attacks. Others prescribe them immediately after a single attack. Most of the time, antihyperuricemic therapy means taking a drug routinely throughout life, which many people find difficult.
Treatment for hyperuricemia that causes no symptoms is not recommended. Asymptomatic hyperuricemia often does not lead to gout or other health problems. In addition, the drugs used to treat it are expensive and carry certain risks. In unusual circumstances treatment may be justified, for example in patients with very high uric acid levels that threaten the kidney or those with a personal or strong family history of gout, kidney stones, or kidney damage.
Before treatment, some experts recommend a 24-hour urine collection sample in patients with frequent gout attacks to determine whether they are over-producers or under-excreters of uric acid. Also, before starting one of these drugs, any previous acute attack should be completely controlled and the joints should not be inflamed. Some health care providers prefer to wait about a month after an attack.
Low doses of NSAIDs or colchicine are used during several months after introducing anti-hyperuricemic therapies to prevent gout attacks. It should be noted that NSAIDs, particularly aspirin and similar drugs, reduce the effectiveness of uricosurics. These are drugs given to under-excreters of uric acid (see below). Patients taking uricosurics should avoid NSAIDs, if possible.
Long-term treatment of hyperuricemia may be recommended for people who have:
- A risk for tophaceous gout
- Had more than two or three acute attacks of gout in the past, particularly if the attacks have not responded promptly to treatment
- Unusually severe attacks, or attacks that affect more than one joint
- Joint damage from gout, as shown on x-rays
- Uric acid kidney stones
- Evidence of kidney damage due to elevated uric acid levels
- Hyperuricemia caused by an identifiable inborn metabolic deficiency
- An inability to use the medications used to treat acute gout
Uricosurics. These drugs prevent the kidney from reabsorbing uric acid, and therefore increase the amount excreted in the urine. They may be used when the kidneys are not eliminating (excreting) enough uric acid, which is present in about 80% of gout cases. Your doctor will check a 24-hour urine to diagnose this problem. They are not used for patients with reduced kidney function or those with tophaceous gout.
Other individuals who may benefit from uricosurics include:
- Those under 60 years of age
- Those with normal diets
- Those who have normal kidney function
- Those who have no risk of kidney stones
Probenecid (Benemid, Probalan) and sulfinpyrazone (Anturane) are the standard uricosurics. A more potent uricosuric, benzbromarone, may work for people with severe tophaceous gout and kidney impairment when other drugs do not. Because benzbromarone can cause liver failure in some patients, it is available in the U.S. only with special authorization.
Probenecid is taken two to three times a day, and sulfinpyrazone begins at twice a day and increases to three or four times daily. The initial doses should be low and gradually increased. Probenecid combined with colchicine is more effective than probenecid alone, but people respond differently, so the dose should be carefully individualized.
The possible side effects of probenecid and sulfinpyrazone include skin rashes, gastrointestinal problems, anemia, and kidney stone formation. To help reduce acidity and the risk for kidney stones, patients should drink plenty of fluids (ideally water, not caffeinated beverages). Sodium bicarbonate supplemented by acetazolamide can also reduce acidity and the risk for stones.
NSAIDs, particularly aspirin, as well as other salicylate drugs, interfere with uricosuric drugs and reduce effectiveness. Patients who need minor pain relief should instead take acetaminophen (Tylenol). Uricosurics interact with many other drugs, and a patient should be sure to inform their health care provider of all medications they are taking.
Probenecid combined with allopurinol (another type of medicine that lowers uric acid levels) is available and may be beneficial in some cases.
Allopurinol (Lopurin, Zyloprim). Allopurinol blocks uric acid production. It is the drug most often used in long-term gout treatment for older patients and those who overproduce uric acid.
Allopurinol is taken by mouth once a day in doses of 100 - 600 mg, depending on the patient's response to treatment. When it is first used, allopurinol can trigger further attacks of gout. Therefore, during the first months (or longer) of therapy, the patient also takes an NSAID or colchicine to reduce that possibility.
Allopurinol has positive effects on "bad" cholesterol levels, so it may be better than other drugs for patients with both gout and coronary artery disease.
Side effects, which can be severe, include:
- Rash
- Diarrhea
- Headache
- Fever
- Leukopenia (a reduction in the number of white blood cells)
- Thrombocytopenia (a reduction in the number of platelets)
- Cataracts
In rare cases, the rash can become severe and widespread enough to be life threatening (this condition is called toxic epidermal necrolysis, or TEN). Allergic individuals who experience only a mild rash may be able to build up their tolerance for the drug by undergoing a desensitization process.
Allopurinol interacts with certain other drugs, such as azathioprine.
Febuxostat. Febuxostat is the first oral drug to emerge in many decades as a new treatment for chronic gout. Approved by the FDA in 2009, it will be particularly useful for patients who are allergic to allopurinol. It is structurally distinct from allopurinol, but, like the older drug, it reduces uric acid production by inhibiting xanthine oxidase. For some patients, gout may flare up after starting the medication, then begin to resolve. The FDA continues to assess its potential for hypersensitivity. It is much more expensive than allopurinol.
Krystexxa. The FDA approved Krystexxa (pegloticase) IV injections for the treatment of gout in September 2010. Injections are given every two or four weeks and are reserved for patients with severe chronic gout who have not been helped by first line treatments. Krystexxa is an enzyme, or biologic, that targets uric acid directly by transforming it into a different molecule which is removed through the urine. In studies, up to 25% of patients experienced allergic reactions ranging from mild to severe. The FDA recommends that an antihistamine and corticosteroid be given prior to the injection to prevent reactions. Side effects, which can be severe, may include rash or hives, shortness of breath, nausea and vomiting, constipation, chest pain, redness and itching, wheezing, swelling of lips or tongue, blood pressure changes, or anaphylactic shock. It has not been tested in patients with heart failure.
Colchicine. colchicine is sometimes prescribed along with allopurinol or probenicid for its preventive and anti-inflammatory effects in cases of severe chronic gout.
Rasburicase. Rasburicase helps to convert uric acid into another molecule, allantoin. It is not appropriate for the average gout patient. It is sometimes given to adults and children receiving cancer treatment to help prevent high uric acid levels from developing. It is given as a single course of intravenous treatment. Side effects may include confusion, dizziness, fatigue, blue lips, light-headedness, shortness of breath, mouth sores, seizures, pale/yellow skin, dark urine, or irregular heart rate.
Warning Note on Drug Treatments for Gout
It should be noted that many drugs used for gout can also precipitate acute gout symptoms and so should not be used until symptoms have subsided. The patient should then start treatment with small doses that gradually increase.
Other Medications
Hypertensive Agents. People with gout have a higher risk for high blood pressure. Some of the drugs used to treat hypertension, such as thiazide diuretics, can increase the risk for gout attacks. Newer agents, such as losartan (an angiotensin II receptor antagonist) and amlodipine (a calcium channel blocker), may have beneficial effects on both high blood pressure and gout.
Data on the safety and effectiveness of combination drug therapies for gout is limited.
Other Treatments
Surgery. Large tophi that are draining, infected, or interfering with the movement of joints may need to be surgically removed. When infection is present, the procedure carries a high risk for complications. People most likely to have surgery also tend to have other medical conditions that might worsen their outlook. In one study, experts suggested that better preventive measures, such as the use of allopurinol, could reduce the need for surgery.
Several other surgical procedures are available for relieving pain and improving the function of affected joints. It is sometimes necessary to replace joints.
Hot and Cold Therapy. Rest and protecting the affected joint with a splint can also promote recovery. Both ice packs and the application of warmth have been found to relieve symptoms.
Lifestyle Changes
Any activities that increase energy demands on the body also increase metabolism of purines, which produces uric acid. Avoiding stress and staying healthy are important for the prevention of attacks.
Dietary Recommendations
Because uric acid levels are only mildly affected by diet, dietary therapy does not play a large role in the prevention of gout. Still, people who have had an attack of gout may benefit from reducing their intake of purine-rich foods, particularly if they eat unusually large quantities of such foods.
While meat and certain types of seafood and shellfish do produce high levels of purines in the blood, research has suggested that not all purine-rich foods are associated with gout. Eating a moderate amount of purine-rich vegetables (spinach, cauliflower, mushrooms, legumes) does not appear to increase the risk of gout.
Dairy products, especially low-fat products (low-fat yogurt and skim milk), may actually protect against gout. Researchers have also found that taking 500 mg a day of vitamin C significantly reduces uric acid levels. They are investigating whether vitamin C can be used to prevent or treat gout.
Foods to Limit or Avoid:
- Organ meats (liver, kidneys, and sweetbreads)
- Red meat (beef, pork, and lamb)
- Meat extracts (soup, broth, and gravies)
- Seafood (anchovies, sardines, herring, fish roe, canned tuna fish, shrimp, lobster, scallops, and mussels)
- Yeast products (beer and baked goods)
Maintain Healthy Weight
A supervised weight-loss program may be a very effective way to reduce uric acid levels in overweight patients. Crash dieting, on the other hand, is counterproductive because it can increase uric acid levels and may cause an acute attack.
Fluids & Alcohol
Drinking plenty of water and other nonalcoholic beverages helps remove uric acid from the body.
It is wise to avoid large amounts of alcohol that promote purine metabolism and uric acid production. Alcohol may also reduce excretion of uric acid. Avoid heavy drinking, especially binge drinking of beer or distilled spirits.
Fructose-rich diets, including soda and fruit juice, may increase the risk of gout in men and women.
Medications
Medications to treat other conditions can increase uric acid levels. Certain diuretics and low dose daily aspirin for instance can affect uric acid levels. Switching to alternative therapies may be necessary.
Avoid Joint Injury
People with gout should also attempt to avoid activities that cause repetitive joint trauma, such as wearing tight shoes.
Preventing an Attack During Travel
Travel is an example of an activity that increases the risk of gout attacks. It not only increases stress, but eating and drinking patterns may change. Before traveling, patients should discuss preventive measures with their health care providers. The doctor may prescribe a prednisone tablet to be taken immediately at the first sign of a gout attack. In most cases, this stops the episode.
Complications
Properly treated gout rarely poses a long-term health threat, though it can be a cause of short-term pain and incapacity for thousands of Americans.
Pain and Disability
Left untreated, gout can develop into a painful and disabling chronic disorder. Persistent gout can destroy cartilage and bone, causing irreversible joint deformities and loss of motion. Survey results released in 2006 show that two-thirds of persons with gout consider the pain of attacks among the worst they've ever experienced. An estimated 75% of those surveyed said flare-ups made walking very difficult, and about 70% reported trouble putting on shoes or playing sports.
Tophi are firm chalky, gritty clumps of uric acid crystals that build up in tissue surrounding a joint. If gout is not treated, tophi can grow to the size of golf balls and can destroy bone and cartilage in the joints, similar to the process in rheumatoid arthritis. If they lodge in the spine, tophi can cause serious damage including compression, although this is very rare. In extreme cases, joint destruction results in complete disability.
Kidney Conditions
Kidney Stones. Kidney stones occur in 10 - 40% of gout patients, and can occur at any time after the development of hyperuricemia. Although the stones are usually composed of uric acid, they may also be mixed with other materials.
Kidney Disease. About 25% of patients with chronic hyperuricemia develop progressive kidney disease, which sometimes ends in kidney failure. It should be noted, however, that many experts believe that chronic hyperuricemia is unlikely to be a common cause of kidney disease. In most cases, the kidney disease comes first and causes high concentrations of uric acid.
Gout and Heart Disease
Gout is found in higher rates in people with high blood pressure, coronary artery disease, and heart failure. Hyperuricemia, in fact, has been associated with a higher risk of death from heart conditions. Studies also found an association between gout and having the metabolic syndrome -- a collection of problems, such as abdominal obesity, high blood pressure, high triglycerides levels, and low "good" cholesterol levels. This syndrome increases a person's risk of heart disease and diabetes.
According to some studies, hyperuricemia may be associated with heart disease, but there are not enough data to confirm such an association.
Other Medical Conditions Associated with Gout
The following are some conditions that are associated with long-term gout:
- Cataracts
- Dry eye syndrome
- Complications in the lungs (in rare cases, uric acid crystals occur in the lungs)
Resources
- www.niams.nih.gov -- National Institute of Arthritis and Musculoskeletal and Skin Diseases
- www.rheumatology.org -- American College of Rheumatology
- www.arthritis.org -- The Arthritis Foundation
- www.gouteducation.org -- The Gout & Uric Acid Education Society
References
Choi HK, Ford ES, Li C, Curhan G. Prevalence of the metabolic syndrome in patients with gout: the Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2007;57(1):109-15.
Choi HK, Willett W, Curhan G. Fructose-rich beverages and risk of gout in women. JAMA. 2010;304(20):2270-8.
Doghramji PP, Edwards NL, McTigue J. Managing gout in the primary care setting: what you and your patients need to know. Am J Med. 2010 Aug;123(8):S2.
Janssens HJ, Fransen J, van de Lisdonk EH, van Riel PL, van Weel C, Janssen M. A diagnostic rule for acute gouty arthritis in primary care without joint fluid analysis. Arch Intern Med. 2010 Jul 12;170(13):1120-6.
Keith MP, Gilliland WR. Updates in the management of gout. Am J Med. 2007;120(3):221-224.
Krishnan E, Baker JF, Furst DE, Schumacher HR. Gout and the risk of acute myocardial infarction. Arthritis Rheum. 2006 Aug;54(8):2688-96.
Neogi T. Clinical practice. Gout. N Engl J Med. 2011;364(5):443-52.Review.
Richette P, Bardin T. Gout. Lancet. 2010 Jan 23;375(9711):318-28.
Sundy JS, Baraf HS, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory toconventional treatment: two controlled trials. JAMA. 2011;306(7):711-20.
Underwood M. Diagnosis and management of gout. BMJ. 2006;332(7553):1315-9.
Wilson JF. In the clinic. Gout. Ann Intern Med. 2010 Feb 2;152(3):ITC21. Review. Erratum in: Ann Intern Med. 2010 Apr 6;152(7):479-80.
Wortmann R. Gout and Hyperuricemia. In: Firestein. Kelley's Textbook of Rheumatology. 8th ed. Philadelphia, Pa: Saunders Elsevier; 2008:chap 87.
Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part I: Diagnosis. Report of a task force of the Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2006;65(10):1301-11.
Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part II: Management. Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2006;65(10):1312-24.
|
Review Date:
1/10/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |








