Knee joint replacement
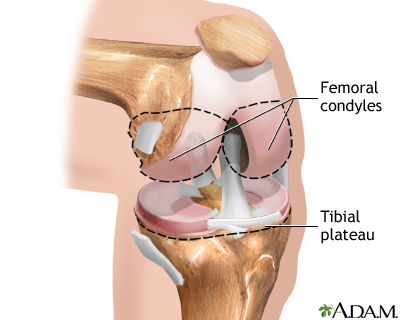
| Normal anatomy |
|
The knee is a complex joint that is made up of the lower end of the thigh bone, or femur (the femoral condyles), and the upper end of the shine bone, or tibia (the tibial plateau). The femoral condyles usually glide smoothly on the tibial plateau, allowing for smooth, painless motion of the lower leg. |
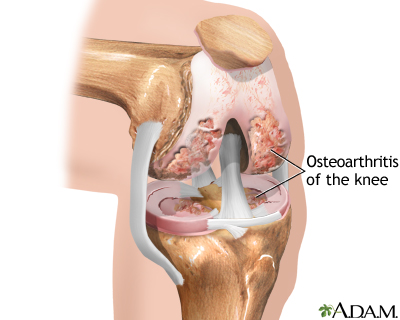
| Indications |
The most common cause of knee damage requiring knee replacement is osteoarthritis, which is a degenerative disease of the cartilage and bones of the knee that cause the surfaces of the knee joint to become irregular and rough, preventing smooth painless motion of the knee.
Knee joint replacement may be recommended for:
- Knee arthritis, which causes knee pain that has failed to respond to conservative therapy (medication and physical therpay for 6 months or more)
- Decreased knee function caused by arthritis
- Inability to work because of knee pain
- Inability to sleep through the night because of knee pain
- Inability to walk more than 3 blocks because of knee pain
- Loosening of a previous knee replacement
- Some knee fractures
|
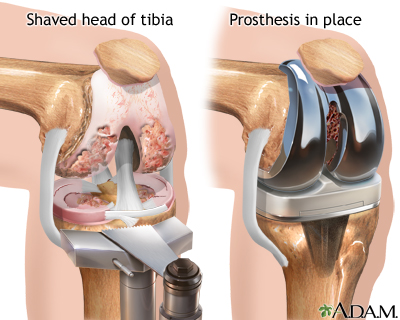
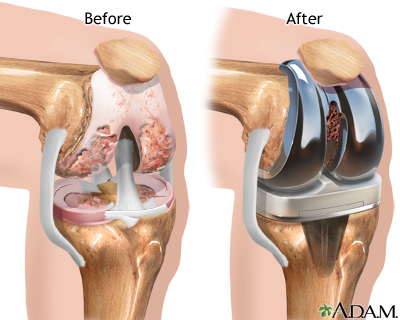
| Procedure |
| The operation is performed under general anesthesia. The orthopedic surgeon makes an incision over the affected knee.
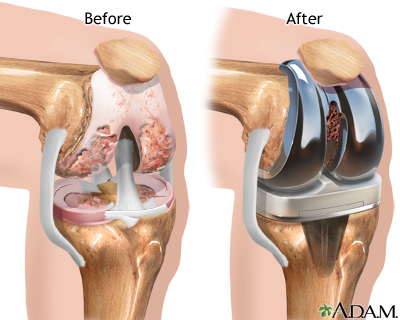
The patella (knee cap) is removed, and the heads of the femur and tibia are shaved to eliminate any rough parts and to permit a better adhesion of the prosthesis. The two parts of the prosthesis are implanted into the thigh bone and the tibia bone using a special bone cement.
|
| Aftercare |
 You will return from surgery with a large dressing over the knee area. A small drainage tube will be placed during surgery to help drain excess fluids from the joint area. Your leg will be placed in a continuous passive motion (CPM) device (a mechanical device that flexes (bends) and extends (straightens) the knee at a pre-set rate and amount of flexion). Gradually, the rate and amount of flexion will be increased as tolerated. The leg should always be in this device while you are in bed. The CPM device helps speed recovery, decreases post-operative pain, bleeding and infection. You will experience moderate pain after surgery. However, you may receive patient-controlled analgesia (PCA), or epidural analgesics to control your pain for the first 3 days after surgery. The pain should gradually decrease, and by the third day after surgery, oral analgesic medications may be sufficient to control your pain. Try to schedule your pain medications about one half hour before walking or position changes. You will also return from surgery with several IV lines in place to provide hydration and nutrition. The IV will remain in place until you are taking adequate amounts of oral fluids. Prophylactic (preventive) antibiotics may be given to reduce the risk of developing an infection, and anticoagulants ("blood thinners") may be administered to prevent blood clots. You may also return from surgery wearing anti-embolism stockings or an inflatable pneumatic compression stockings. These devices are used to reduce your risk of developing blood clots, which are more common after lower extremity surgery. Additionally, you will be encouraged to start moving and walking early after surgery. You will be assisted out of bed to a chair on the first day after surgery. When in bed, bend and straighten your ankles frequently to prevent development of blood clots.
|

|
Review Date:
5/21/2012
Reviewed By:
Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997-
A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.