Fibromyalgia
Highlights
Diagnosis
- Fibromyalgia can be difficult to diagnose. It can take 5 years for the average person with the condition to finally get a diagnosis. As many as three out of every four people with fibromyalgia remain undiagnosed.
Treatment
- Exercise, especially when combined with cognitive behavior therapy (CBT), can help people with fibromyalgia feel better.
Introduction
Fibromyalgia is a condition that causes lasting, and sometimes debilitating muscle pain and fatigue. No one knows exactly what causes it, but it may be triggered by injuries, emotional trauma, or viral infections. Fibromyalgia is also known as fibrositis or fibromyositis.
General Description of Fibromyalgia Symptoms
Pain. The main symptom of fibromyalgia is pain. The pain can be in one place or all over the body. The exact locations of the pain are called tender points. Fibromyalgia pain is often described as:
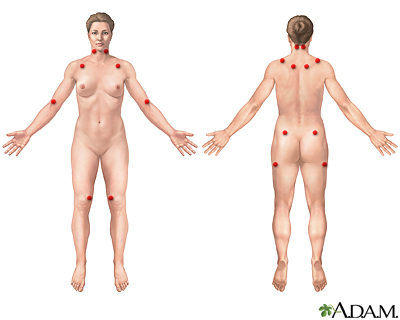
- Tender point pain that occurs in local areas. People who are diagnosed with fibromyalgia feel pain in at least 11 of 18 specific tender points. Pain starts in the muscles, usually in the neck and shoulders, and then spreads out from these areas. The joints are not affected, although many patients feel like the pain is starting in their joints. There are no lumps with the pain points, and no signs of inflammation (swelling). The skin also feels more sensitive to the touch.
- Widespread stiffness, burning, and aching pain. The pain also "radiates," or spreads, to nearby areas. Most patients report feeling some pain all the time, but the intensity of the pain may increase or decrease. Many describe it as "exhausting." The pain can vary with the time of day, changes in the weather, physical activity or inactivity, and stress. The pain is often more intense when sleep is disturbed.
Fatigue and Sleep Disturbances. Fatigue and sleep disturbances are almost universal in patients with fibromyalgia. Restless legs syndrome (RLS) and periodic limb movement disorder (PLMD) are also common. It is not clear whether fibromyalgia leads to poor sleeping patterns or if the sleep disturbances come first.
Many patients complain that they can't get to sleep or stay asleep, and they feel tired when they wake up. Some report that their fatigue is more distressing than their pain, because it interferes with their ability to enjoy life. Some experts believe that if a person does not have sleep problems, the condition may not be fibromyalgia.
Researchers condtinue to investigate the link between fibromyalgia and sleep.
Depression and Mood. Up to a third of fibromyalgia patients have depression. Disturbances in memory and concentration are also very common. These conditions often go undiagnosed.
Other Symptoms. The following symptoms may also occur with fibromyalgia:
- Digestive problems, including irritable bowel syndrome with gas, and alternating diarrhea and constipation
- Dizziness
- Dry mouth
- Painful menstrual periods
- Problems with balance
- Tension or migraine headaches
- Tingling or numbness in the hands and feet
- Urinary frequency caused by bladder spasms
Symptoms in Children. In general, children with fibromyalgia most often have sleep disorders and widespread pain. They may also experience fatigue, stress, depression, and headaches.
Causes
In the most common type of fibromyalgia, the cause is unknown. Physical injuries, emotional trauma, or viral infections may trigger the disorder, but no one trigger has been proven to cause primary fibromyalgia.
Many experts believe that fibromyalgia is not a disease, but is rather a chronic pain condition brought on by several abnormal body responses to stress. Areas in the brain that are responsible for the sensation of pain react differently in fibromyalgia patients than the same areas in healthy people.
People with fibromyalgia have decreased activity in opioid receptors in parts of the brain that affect mood and the emotional aspect of pain. This reduced response might explain why fibromyalgia patients are likely to have depression, and are less responsive to opioid painkillers.
Brain Chemicals and Hormonal Abnormalities
Many hormonal, metabolic, and brain chemical abnormalities have been described in studies of fibromyalgia patients. Changes appear to occur in several brain chemicals, although no regular pattern has emerged that fits most patients. Fibromyalgia may be a result of the effects of pain and stress on the central nervous system that lead to changes in the brain, rather than a brain disorder itself.
Serotonin. Of particular interest to researchers is serotonin, an important nervous system chemical messenger found in the brain, gut, and other areas of the body. Serotonin helps create feelings of well-being, adjusts pain levels, and promotes deep sleep. Lower serotonin levels have been noted in some patients with fibromyalgia.
Stress Hormones. Researchers have also found abnormalities in the hormone system known as the hypothalamus-pituitary-adrenal gland (HPA) axis. The HPA axis controls important functions, including sleep, the stress response, and depression. Changes in the HPA axis appear to produce lower levels of the stress hormones norepinephrine and cortisol. Lower levels of stress hormones lead to impaired responses to psychological or physical stresses. (Examples of physical stress include infection or exercise.)
Certain factors may inappropriately trigger a person's stress response and contribute to the development of fibromyalgia, including:
- Infections (Epstein-Barr virus, Lyme disease)
- Physical trauma (such as a car accident)
- Emotional stress
- Hormonal changes (such as an underactive thyroid gland)
- Medications
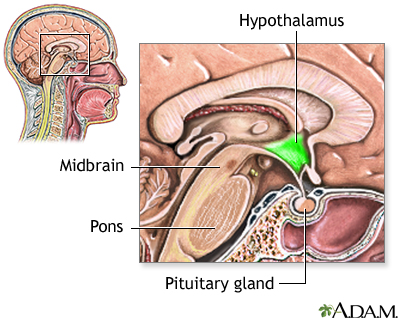
Low IGF-1 Levels. Some studies have reported low levels of insulin-like growth factor-1 (IGF-1) in about a third of fibromyalgia patients. IGF-1 is a hormone that promotes bone and muscle growth. Low levels of growth hormone may lead to impaired thinking, lack of energy, muscle weakness, and intolerance to cold. Studies suggest that changes in growth hormone likely stem from the hypothalamus in the brain. Although researchers have not found a link between IGF-1 levels and fibromyalgia, growth hormone levels in the blood may be a marker of the disorder.
Abnormal Pain Perception and Substance P. Some studies have suggested that people with fibromyalgia may perceive pain differently than healthy people. Fibromyalgia may involve too much activity in the parts of the central nervous system that process pain (the nociceptive system). Brain scans of fibromyalgia patients have found abnormalities in pain processing centers. For example, researchers have detected up to three times the normal level of substance P (a chemical messenger associated with increased pain perception) in fibromyalgia patients.
Some fibromyalgia patients may be oversensitive to external stimulation, and overly anxious about the sensation of pain. This increase in awareness is called generalized hypervigilance. Fibromyalgia patients have been found to have greater awareness of, or less tolerance for, movement problems (such as tremor) that don't match their expected sensory feedback. This mismatch in sensory signals might enhance the perception of pain. Fibromyalgia patients also seem to be more sensitive to sounds.
Immune Abnormalities
Fibromyalgia has symptoms that resemble those of some rheumatic illnesses, including rheumatoid arthritis and lupus (systemic lupus erythematosus). These are autoimmune diseases in which a defective immune system mistakenly attacks the body's own healthy tissue, producing inflammation and damage. The pain in fibromyalgia, however, does not appear to be due to autoimmune factors, and there is little evidence to support a role for an inflammatory response in fibromyalgia.
Psychological and Social Effects
Psychological and social factors are not primary causes of fibromyalgia, but they may contribute to the condition in three ways:
- They could make people more susceptible to fibromyalgia.
- They may play some role in triggering the onset of the condition.
- They may perpetuate the condition.
Studies have reported higher rates of severe emotional and physical abuse in patients with fibromyalgia compared with the general population. Most often, the abusers are family members or partners. A history of sexual abuse does not seem to be a risk factor for fibromyalgia. However, women who have been raped may face an increased risk for the disease.
Post-traumatic stress disorder (PTSD) or chronic stress may play a strong role in the development of fibromyalgia in some patients. PTSD, an anxiety disorder, is a reaction to a specific traumatic event. Some evidence indicates that PTSD actually causes changes in the brain, possibly from long-term overexposure to stress hormones.
Muscle Abnormalities
Some research has found muscle abnormalities in fibromyalgia patients, including:
- Biochemical abnormalities: Fibromyalgia patients may have lower levels of the muscle-cell chemicals phosphocreatine and adenosine triphosphate (ATP). These chemicals regulate the level of calcium in muscle cells. Calcium is an important component in the muscles' ability to contract and relax. If ATP levels are low, calcium is not "pushed back" into the cells, and the muscle remains contracted.
- Functional abnormalities: The pain and stress of the disease itself may harm muscle function.
- Structural and blood flow abnormalities: Some researchers have seen overly thickened capillaries (tiny blood vessels) in the muscles of fibromyalgia patients. The abnormal capillaries could produce lower levels of compounds essential for muscle function, as well as reduce the flow of oxygen-rich blood to the muscles.
To date, none of these abnormalities has a clearly defined relationship with fibromyalgia.
Risk Factors
About 5 million Americans, or 2% to 5% of adults have fibromyalgia. The condition affects women more often than men.
Some evidence suggests that several factors may make people more susceptible to fibromyalgia. These risk factors include:
- Being female
- Coming from a very stressful culture or environment
- Having a psychological vulnerability to stress
- Having had difficult experiences in childhood
Women
Nine out of 10 fibromyalgia patients are women. Women may be especially likely to develop fibromyalgia during menopause.
Age
The disorder usually occurs in people ages 20 - 60, though it can start at any time. Some studies have noted peaks at around age 35. Others note that fibromyalgia is most common in middle-aged women. In one study, cases of fibromyalgia increased with age and reached a frequency of more than 7% among people in their 60s and 70s.
Juvenile Primary Fibromyalgia. This type of fibromyalgia appears in adolescents, more commonly in girls. It typically starts after age 13 and peaks at age 14. Juvenile primary fibromyalgia is uncommon, but studies indicate that its incidence may be increasing. Symptoms are similar to those of adult fibromyalgia, but outcomes may be better in young people.
Family Factors
Studies report an increased prevalence of fibromyalgia among family members. Children and siblings of people with fibromyalgia are eight times more likely to develop the condition than the general population. Family members are also more sensitive to pain, and more likely to have related conditions such as irritable bowel syndrome, temporomandibular disorder, or headaches.
Genetic, environmental, and psychological factors may all be involved in fibromyalgia. Current research is examining variations in certain genes in people with fibromyalgia. These changes involve the stress response and may affect the way a person processes pain.
Diagnosis
It is important to diagnose fibromyalgia as soon as possible, so treatment can be started. But because there is no clear method (such as laboratory or imaging tests) to diagnose the condition, as many as three out of every four people with fibromyalgia remain undiagnosed. It can take an average of 5 years to finally get a diagnosis.
Fibromyalgia criteria can be helpful, particularly if the patient does not have another disorder, such as depression or arthritis, which could complicate the diagnosis. Failure to meet the criteria, however, does not rule out fibromyalgia. Fibromyalgia should be suspected in any person who has muscle and joint pain with no identifiable cause.
Because many patients do not meet the current fibromyalgia criteria, the American College of Rheumatology (ACR) has proposed introducing a new set of diagnostic criteria that take into consideration symptoms such as fatigue, sleep disturbances, and cognitive problems, in addition to pain.
Criteria for Classifying Fibromyalgia
In 1990, the ACR set the following criteria for classifying fibromyalgia:
A. Widespread pain must be present for at least 3 months. This pain must appear in all of the following locations:
- Both sides of the body
- Above and below the waist
- Along the length of the spine
B. Pain in at least 11 of 18 specific areas called tender points on the body. When the doctor presses on a tender point, the pain is very localized and intensely painful (not just tender). Tender points are located in the following areas:
- The left or right side of the back of the neck, directly below the hairline
- The left or right side of the front of the neck, above the collarbone (clavicle)
- The left or right side of the chest, right below the collarbone
- The left or right side of the upper back, near where the neck and shoulder join
- The left or right side of the spine in the upper back between the shoulder blades (scapula)
- The inside of either arm where it bends at the elbow
- The left or right side of the lower back, right below the waist
- Either side of the buttocks below the hip bones
- Either kneecap
New criteria. The ACR's proposed new criteria would replace the tender point examination with a widespread pain index (WPI), which counts the number of areas where the patient has felt pain in the last week. It would also include a symptom severity scale (SSS), which rates on a scale of 0 to 3 the severity of three common fibromyalgia symptoms:
- Fatigue
- Unrefreshing sleep
- Cognitive symptoms
Another three points can be added for these additional symptoms:
- Numbness
- Dizziness
- Nausea
- Irritable bowel syndrome
- Depression
The WPI and SS scores are totaled to create a final score of between 0 and 12. To meet the criteria for a fibromyalgia diagnosis, a patient would need to have seven or more pain areas and a symptom severity score of five or more; or three to six pain areas and a symptom severity score of nine or more. The symptoms must have been present for at least 3 months.
Medical and Personal History
A doctor should always take a careful personal and family medical history, which includes a psychological profile and history of any factors that might indicate other conditions, such as:
- Infectious diseases
- Muscle weakness
- Physical injuries
- Rashes
- Recent weight change
- Sexual, physical, or substance or alcohol abuse
During this medical history, patients should tell the doctor about any drugs they take, including vitamins and over-the-counter or herbal medications.
Physical Examination
The physical exam may not reveal much, other than the tender spots that are included in the diagnostic criteria. These spots must be painful when pressed, not simply tender. For fibromyalgia to be diagnosed, these tender sites should not show signs of inflammation (redness, swelling, or heat in the joints and soft tissue).
The tender points may change in location and sensitivity over time. A doctor may recheck tender points that do not respond the first time in patients who have other fibromyalgia symptoms.
The health care provider will also examine the nails, skin, mucus membranes, joints, spine, muscles, and bones to help rule out arthritis, thyroid disease, and other disorders.
Other Tests
No blood, urine, or other laboratory tests can definitively diagnose fibromyalgia. If these tests show abnormal results, the doctor should look for other disorders.
Tests that are done to diagnose diseases with similar symptoms may include:
- Antibody tests
- Complete blood count
- C-reactive protein
- Erythrocyte sedimentation rate (ESR)
- Thyroid and liver function tests
The doctor may suggest follow-up psychological profile testing if laboratory results do not indicate a specific disease.
Conditions with Similar Symptoms
Between 10% and 30% of all doctor's office visits are due to symptoms that resemble those of fibromyalgia, including fatigue, malaise, and widespread muscle pain. Because no laboratory test can confirm fibromyalgia, doctors will usually first test for similar conditions.
Getting diagnosed with one of the disorders below may not always rule out fibromyalgia, because several conditions may overlap or coexist with fibromyalgia, and have similar symptoms. Like fibromyalgia, a number of these conditions also cannot easily be diagnosed. It is not clear whether these conditions cause fibromyalgia, are risk factors for the disorder, have causes in common with fibromyalgia, or have no relationship at all with it.
Chronic Fatigue Syndrome. There is a significant overlap between fibromyalgia and chronic fatigue syndrome (CFS). As with fibromyalgia, the cause of CFS is unknown. A doctor can diagnose either disorder based only on symptoms reported by the patient. The two disorders share most of the same symptoms. They are also treated almost identically. The main differences are:
- Pain with tender points is the primary symptom in fibromyalgia. Some patients with CFS exhibit similar tender pressure points; however, their muscle pain is less prominent.
- Fatigue is the main symptom in CFS. It is severe, is not caused by excessive work or exercise, and is not relieved by rest or sleep.
Some doctors believe that fibromyalgia is simply an extreme type of chronic fatigue syndrome. However, evidence indicates that the two disorders are distinct, and each has its own treatments.
Myofascial Pain Syndrome. Myofascial pain syndrome can be confused with fibromyalgia and may also occur with it. Unlike fibromyalgia, myofascial pain tends to occur in trigger points, as opposed to tender points, and typically there is no widespread, generalized pain. Trigger-point pain occurs in tight muscles, and when the doctor presses on these points, the patient may experience a muscle twitch. Unlike tender points, trigger points are often small lumps, about the size of a pencil eraser.
Major Depression. The link between psychological disorders and fibromyalgia is very strong. Studies report that 50 to 70% of fibromyalgia patients have a lifetime history of depression. However, only 18 to 36% of fibromyalgia patients have major depression.
Some studies have found that people who have both psychological disorders and fibromyalgia are more likely to seek medical help, compared with patients who simply have symptoms of fibromyalgia. If this is the case, study results may be biased, finding a higher-than-actual association between depression and fibromyalgia.
Depressed feelings in people with fibromyalgia can be normal responses to the pain and fatigue caused by this syndrome. Such emotions are temporary and related to the condition. They are not considered to be a depression disorder. Unlike ordinary periods of sadness, an episode of major depression can last for many months.
Symptoms of major depression include the following:
- Depressed mood every day
- Feeling worthless or inappropriately guilty
- Inability to concentrate or make decisions
- Insomnia or excessive sleeping
- Low energy every day
- Restlessness or a sense of being slowed down
- Significant weight gain or loss (of 10% or more of a person's typical body weight)
- Suicidal thoughts
If several of the above symptoms are present, and none of the physical symptoms (particularly the tender points) of fibromyalgia exist, the condition is most likely major depression.
Chronic Headache. Chronic primary headaches, such as migraines, are common in fibromyalgia patients. Some experts believe that migraine headaches and fibromyalgia both involve defects in the systems that regulate certain chemical messengers in the brain, including serotonin and epinephrine (adrenaline). Low levels of magnesium have also been noted in patients with both fibromyalgia and migraines. Chronic migraine sufferers who do not benefit from usual therapies may also have fibromyalgia.
Multiple Chemical Sensitivity. Multiple chemical sensitivity (MCS) is a term for conditions in which certain chemicals cause symptoms that are similar to CFS or fibromyalgia. As with CFS and fibromyalgia, MCS may be a medical or psychological problem. Because everyone is exposed to many chemicals on a daily basis, it is very difficult to determine whether chemicals are responsible for specific symptoms.
Experts have come up with criteria to help recognize MCS:
- Symptoms can be produced by exposure to the chemical at levels lower than the person previously or usually tolerated.
- Symptoms can be triggered by multiple substances that are chemically unrelated.
- Symptoms involve multiple organ systems.
- The condition is chronic.
- The symptoms always happen with repeated exposure to a chemical. (These are often common chemicals found in popular products, such as perfumes, fabric softeners, and air fresheners.)
- The symptoms improve when the chemical is removed.
Restless Legs Syndrome. About 15% of people with fibromyalgia have restless legs syndrome (RLS). RLS is an unsettling and poorly understood movement disorder that is sometimes described as a sense of unease and weariness in the lower leg that is aggravated by rest and relieved by movement.
Lyme Disease. Lyme disease is a bacterial disease transmitted by ticks. Health care providers can usually (but not always) diagnose Lyme disease correctly using blood tests that identify antibodies directed at the bacteria that cause it. But if this disorder isn't diagnosed right away or it comes back, it may be mistaken for fibromyalgia. Some experts believe that 15 - 50% of patients referred to clinics for Lyme disease actually have fibromyalgia. If fibromyalgia patients are incorrectly diagnosed and treated for Lyme disease with long courses of antibiotics, the drugs may have serious side effects.
Drugs and Alcohol. Fatigue is a side effect of many prescription and over-the-counter medications, such as antihistamines. Constant fatigue is also a symptom of drug and alcohol dependency or abuse. Health care providers should consider medications as a possible cause of fatigue if a person has recently started, stopped, or changed medications. Withdrawal from caffeine can also produce depression, fatigue, and headache.
Polymyalgia Rheumatica. Polymyalgia rheumatica is a condition that causes pain and stiffness. It generally occurs in older women. Tender points are also present with this disorder, although they almost always occur in the hip and shoulder area. Morning stiffness is common, and patients may also experience fever, weight loss, and fatigue. It is important to diagnose polymyalgia rheumatica early with an erythrocyte sedimentation rate (ESR) test, because some PMR patients have a related condition (giant cell arteritis) that may lead to blindness if not treated. Polymyalgia rheumatica usually responds to low doses of a steroid medication such as prednisone.
Disorders Affected by the Sympathetic (also called Autonomic) Nervous System. Other conditions that commonly occur with fibromyalgia include:
- Chest pain and heart palpitations
- Mitral valve prolapse
- Sudden drop in blood pressure
Certain stress-related disorders are also common with fibromyalgia, and have overlapping symptoms. Some experts believe these disorders interact so often that they may all be part of one general condition. Examples are:
- Irritable bowel syndrome (IBS) -- More than half of patients with fibromyalgia also have IBS, a gastrointestinal disorder that causes cramping, abdominal pain, bloating, constipation, and diarrhea.
- Temporomandibular joint disorders (TMJ) -- TMJ affects the muscles of the face and jaw, leading to pain in those areas. Most fibromyalgia patients also experience face and jaw pain.
- Chemicals and environmental toxins -- exposure to various chemicals and environmental toxins such as solvents, pesticides, or heavy metals (cadmium, mercury, or lead) can cause fatigue, chronic pain, and other symptoms of fibromyalgia.
Prognosis
Fibromyalgia can be mild or disabling, and the emotional toll can be substantial. People with fibromyalgia experience greater psychological distress and a greater impact on quality of life than those with other conditions, such as chronic low back pain.
About half of all patients have difficulty with routine daily activities, or are unable to perform them. An estimated 30 - 40% of patients have had to quit work or change jobs. Patients with either CFS or fibromyalgia are more likely to lose their jobs, possessions, and support from friends and family than are people suffering from other conditions that cause fatigue.
Risk of Negative Behaviors
The pain, emotional consequences, and sleep disturbances that come with fibromyalgia may lead to self-medication and overuse of sleeping pills, alcohol, drugs, or caffeine.
Long-term Outlook
Outlook in Adults. Although fibromyalgia is lifelong, it does not get worse and is not fatal. Some studies show that fibromyalgia symptoms remain stable over the long term, while others report that more than a quarter of patients see improvement in their pain symptoms over time. Studies suggest that regular exercise improves the outlook. People with a significant life crisis or who are on disability have a poorer outcome based on their:
- Ability to work
- Depression
- Disturbed sleep
- Fatigue
- Feelings about their condition
- Pain
Outlook in Children. Children with fibromyalgia tend to have a better outlook than adults with the disorder. Several studies have reported that more than half of children with fibromyalgia recover in 2 to 3 years.
Treatment
Fibromyalgia is a mysterious condition. What causes it, and how it produces damage are still largely unknown. No strong evidence indicates that any single treatment (or combination of treatments) has any significant effect for most patients. Treatment usually involves not only relieving symptoms, but also changing people's attitudes about their disease, and teaching them behaviors that help them cope.
In 2007 pregabalin (Lyrica) became the first drug FDA-approved for the treatment of fibromyalgia. A year later, the FDA approved the drug duloxetine (Cymbalta) for fibromyalgia. Cymbalta has been shown to reduce fibromyalgia pain by more than 30%. The serotonin-norepinephrine reuptake inhibitor (SNRI) milnacipran (Savella) is also approved for this condition.
Many patients with fibromyalgia are treated first with medication; however, the American Pain Society Fibromyalgia Panel recommends a combined approach using cognitive-behavioral therapy, education, medication, and exercise. A combination of non-drug therapies appears to work just as well as drug therapy for improving pain, depression, and disability. This combination includes exercise, stress management, massage, and diet.
Treatments usually involve trial and error:
- Patients may start with physical therapy, exercise, stress reduction techniques, and cognitive-behavioral therapy.
- If these methods fail to improve symptoms, an antidepressant or muscle relaxant may be added to the treatment. Doctors usually prescribe these drugs to improve pain tolerance.
- Patient education and programs that encourage coping skills are an important part of any treatment plan.
Preparation for Treatment
Patients must have realistic expectations about the long-term outlook of their condition, and their own abilities. It is important to understand that fibromyalgia can be managed, and patients can live a full life with the disorder.
The definition of improvement is personal. For example, some patients are pleased with only a 10% reduction in pain and other symptoms.
The following tips may be helpful when starting a fibromyalgia treatment program:
- The goal of therapy is to relieve symptoms, not cure them.
- Treatment must be tailored to each patient, and a combination approach is often needed.
- Patients must begin all treatments with the attitude that they are trial-and-error. No single treatment will necessarily relieve all symptoms.
- Treatments are long-lasting, in some cases lifelong, and patients should not be discouraged by the return of symptoms (relapses).
- Enlisting family members, partners, and close friends, particularly to help with exercise and stretching programs, can be helpful.
- Joining a fibromyalgia support group also helps many patients. Support groups may also help their family members, particularly the parents of children with fibromyalgia.
Lifestyle Changes
Many studies have shown that exercise is the most effective part of managing fibromyalgia, and patients should expect to take part in a long-term exercise program. Physical activity prevents muscle wasting, increases emotional well-being, and, over time, reduces fatigue and pain.
Exercise programs for fibromyalgia often combine aerobic, strength training, and flexibility exercises with self-education. Some studies have shown that improvements can last for up to 9 months after the exercise program ends.
Graded Exercise. The basic approach used for fibromyalgia is called graded exercise. Graded exercise means slowly increasing the amount of physical activity.
In general, graded exercise involves:
- A very gradual program of activity, beginning with mild exercise and building in intensity over time.
- Stretching exercises before working out. A daily stretching routine can help relax tense muscles and prevent soreness.
- Walking, swimming, and using equipment such as treadmills or stationary bikes. Swimming and water therapy are good because they don't require putting weight on the joints.
Adding cognitive behavioral therapy (CBT) to a program of graded exercise may also help people with fibromyalgia feel better.
It is important to start an exercise program slowly. Patients who try difficult exercises too early actually experience an increase in pain, and are likely to become discouraged and quit. Every patient must be prepared for relapses and setbacks, and should not get discouraged. Patients who do not respond to one type of exercise might consider experimenting with another form.
Bursts of Exercise. Exercise can help relieve fibromyalgia, but many people with the condition find it hard to exercise for long periods of time. Research finds that adding small amounts of everyday physical activity like taking the stairs, gardening, and walking helps people with fibromyalgia increase their daily exercise amount, and improves their pain and fatigue. As people improve, they can increase their activity level gradually.
Physical Therapy. Physical therapy can also be very helpful. Studies suggest that physical therapy may reduce muscle overload and fatigue, and strengthen weak muscles.
Tai Chi. The ancient Chinese exercise program that combines slow movement, breathing, and meditation may also help people with fibromyalgia. Tai chi improves pain, fatigue, physical functioning, sleeplessness, and depression, and it does not have any side effects.
Establishing Regular Sleep Routines
Sleep is essential, particularly because sleep disruptions worsen pain. Many patients with fibromyalgia have trouble getting a restful and healing night's sleep. Those who are consistently unable to sleep have little improvement in symptoms. Swing shift work, for example, is extremely hard on fibromyalgia patients. Poor sleep habits can add to sleep problems. Tips for good sleep habits include:
- Avoid caffeine or alcohol 4 - 6 hours before bedtime.
- Avoid drinking fluids right before bedtime so that you do not have to wake up to urinate.
- Avoid exercising 6 hours before bedtime.
- Avoid large meals before bedtime. A light snack, however, may help you sleep.
- Avoid naps, especially in the evening or late afternoon.
- Establish a regular time for going to bed and getting up in the morning. Maintain this schedule even on weekends and during vacations.
- If you are unable to fall asleep after 15 or 20 minutes, go into another room and start a quiet activity. Return to bed when you feel sleepy.
- Minimize light and maintain a comfortable, moderate temperature in the bedroom. Keep the bedroom well ventilated.
- Use the bed only for sleep and sexual relations.
[For more information see In-Depth Report #27: Insomnia.]
Diet
Fibromyalgia patients should maintain a healthy diet low in animal fat and high in fiber, with plenty of whole grains, fresh fruits, and vegetables. Although everyone should be careful about calories from fats, some types of fats are healthy.
Omega-3 Fatty Acids. Oils containing omega-3 fatty acids are of particular interest for arthritic pain. Such oils are found in cold-water fish. You can also purchase these oils as supplements called EPA-DHA or omega 3.

Vegetarian or Vegan Diet. A vegan diet has no meat, dairy, or eggs and includes uncooked fruits, vegetables, nuts, and germinated seeds. The actual benefit of vegetarian and vegan diets for fibromyalgia remains unproven.
Stress Reduction Techniques
Relaxation and stress-reduction techniques are proving helpful for managing chronic pain. Evidence shows that people with fibromyalgia have a more stressful response to daily conflicts and encounters than those without the disorder. Several relaxation and stress-reduction techniques may be helpful for managing chronic pain, including:
- Biofeedback
- Deep breathing exercises
- Hypnosis
- Massage therapy
- Meditation
- Muscle relaxation techniques
Biofeedback. During a biofeedback session, electric leads are taped to a person's head. The person is encouraged to relax using any method that works. Brain waves are measured and an audio signal sounds when alpha waves are detected. Alpha waves are brain waves that occur with a state of deep relaxation. By repeating the process, people using biofeedback connect the sound with the relaxed state, and learn to relax on their own. Evidence from studies does not suggest that biofeedback techniques are very helpful for fibromyalgia patients.
Meditation. Meditation, which has been used for many years in Eastern cultures, is now widely accepted in this country as an effective relaxation technique. A number of studies are reporting its benefits for fibromyalgia patients who practice on a regular basis.
Meditation can provide the following physical benefits:
- Reduced heart rate, blood pressure, adrenaline levels, and skin temperature
- Improved well-being
- Better sleep -- melatonin helps regulate the sleep-wake cycle
- Less pain, possibly from reductions in levels of cortisol, a stress hormone
An important goal for both religious and therapeutic meditation practices is to quiet the mind -- essentially to relax thought. This redirection of brain activity from thoughts and worries to the senses disrupts the stress response and prompts relaxation and renewed energy.
People who try meditation for the first time should understand that it can be difficult to quiet the mind, and they should not be discouraged by a lack of immediate results. Some experts recommend meditating for no longer than 20 minutes in the morning after waking up, and then again in the early evening before dinner. Meditating just once a day is helpful. Do not meditate before going to bed, because it causes some people to wake up in the middle of the night, alert and unable to get back to sleep.
Hypnosis. In one small study, hypnosis was more effective than physical therapy at improving function and reducing pain.
Massage Therapy. Massage therapy is thought to slow the heart and relax the body. In one study, patients who were given 30-minute massage sessions twice a week had lower stress and anxiety and less pain after 5 weeks compared to a group receiving an alternative therapy called transcutaneous electrical stimulation (TENS).
Alternative Treatments
Because of the difficulties in treating fibromyalgia, many patients seek alternative therapies. Although some studies have reported a benefit from these treatments, there is not enough evidence to recommend them.
Acupuncture. Studies continue to report conflicting results on acupuncture's ability to relieve pain. Several small studies suggest that it offers some benefit, especially to people who cannot take medicines because of side effects. Acupuncture also seems to help relieve pain when added to treatment with tricyclic antidepressants and exercise, and the improvements last for a few months after treatment ends. Other studies have not found enough evidence to support the use of acupuncture for fibromyalgia.
Chiropractic or Osteopathic Manipulation. Chiropractic or osteopathic manipulation may also help some patients. Osteopathic techniques may include manipulation of the spine or muscle tissue release. While some studies have reported pain relief and improved sleep with osteopathic manipulation, larger and better designed studies are needed to clearly identify whether this is an effective treatment. There is always a very small risk for side effects from any of these techniques. For example, in rare cases manipulation of the neck has caused a stroke or damage to the large blood vessels in the neck.
Herbs and Supplements
Some alternative remedies are being investigated for fibromyalgia. Examples include: melatonin, a natural hormone associated with the sleep-wake cycle; and S-adenosylmethionine (SAMe), a natural substance that has antidepressant, anti-inflammatory, and pain relieving properties. Studies have shown benefits for some patients with fibromyalgia, but trials done so far have not been well designed.
Generally, manufacturers of herbal remedies and dietary supplements do not need approval from the U.S. Food and Drug Administration to sell their products. It is extremely important for patients to realize that any herbal remedy or natural medicine that has positive effects most likely has negative side effects and toxic reactions, just as like any conventional drug. There have been a number of reported cases of serious and even deadly side effects from herbal products.
Consult a doctor before using any herbal products or dietary supplements. Also discuss with your doctor the potential interactions between the supplements and any medications you take.
Behavioral Therapy
Studies show that fibromyalgia patients feel better when they deal with the consequences of the disorder on their lives. Cognitive-behavioral therapy (CBT) is an effective way to help patients deal with chronic pain and stressful situations. Evidence suggests that CBT can help some patients with fibromyalgia.
Although the effects of CBT and other non-medication treatments for fibromyalgia do not always last over the long-term, they may help certain groups of people, particularly those with a high level of psychological stress.
CBT may be particularly useful for addressing insomnia, one of the hallmark symptoms of fibromyalgia. In studies, patients who received CBT for insomnia woke up less often at night, had fewer symptoms of insomnia, and had an improved mood.
The Goals of CBT. The primary goals of CBT are to change mistaken ideas and self-defeating behaviors. Patients learn to think of pain as something other than a negative factor that controls their life. Over time, the idea that they are helpless goes away and they learn that they can manage the pain.
CBT is particularly helpful for defining and setting limits, which is extremely important for fibromyalgia patients, who often push themselves too far. Patients learn to prioritize their responsibilities and drop some of the less important tasks or delegate them to others. Learning these coping skills can eventually lead to a more manageable life. Patients also learn to view themselves and others with a more flexible attitude.
How CBT Works. CBT usually consists of 6 to 20 one-hour sessions. Patients also receive homework, which usually includes keeping a diary and trying tasks they have avoided in the past because of negative attitudes.
A typical CBT program may involve the following measures:
- Keeping a Diary. Patients are usually asked to keep a diary. The diary serves as a guide for setting limits and planning activities. Patients use the diary to track any stress, such as a job or relationship that may be worsening their pain.
- Confronting Negative or Discouraging Thoughts. Patients are taught to challenge and reverse negative beliefs. For example, "I'm not good enough to control this disease, so I'm a total failure" becomes the coping statement, "I can learn to control this disease."
- Setting Limits. Limits are designed to keep both mental and physical stress within manageable levels, so that patients do not get in over their heads and become discouraged. For example, tasks are broken down into incremental steps, and patients focus on doing one step at a time.
- Seeking out Pleasurable Activities. Patients list a number of enjoyable low-energy activities that they can conveniently schedule.
- Prioritizing. Patients learn to drop some of the less critical tasks or delegate them to others.
Patients should learn to accept that relapses occur, and that over-coping and accomplishing too much too soon can often cause a relapse. Patients should respect these relapses and back off. They should not consider them a sign of failure.
Research also shows that patient education can be effective in treating fibromyalgia, especially when combined with CBT, exercise, and other therapies. Educational programs can take the form of group discussions, lectures, or printed materials, although there isn't any clear evidence that one type of education works best.
Treatment of Fibromyalgia in Children
Experts say the treatment of fibromyalgia in children should begin with non-drug therapies, including exercise and cognitive behavioral therapy. Medications such as pregabalin and milnacipran are recommended for adults, but they have not been well tested in children. Analgesics and NSAIDs are not very effective in children. Psychological therapies may help control pain in children, although there is no evidence that they improve disability or mood.
Support Organizations and Group Therapy
Cognitive therapy may be expensive and often is not covered by insurance. Other effective approaches that are free or less costly include support groups or group psychotherapy. The success of these programs varies based on the skill of the therapist.
Medications
Pregabalin (Lyrica), duloxetine (Cymbalta), and milnacipran (Savella) are approved specifically for treating fibromyalgia. However, many other drugs, including antidepressants, sleeping aids, pain relievers, and muscle relaxants, are also used to treat the condition. The goal with medication is to improve sleep and pain tolerance. There is no consensus over which treatment is most useful, or whether a combination of treatments works best. Patients may receive drug treatments in combination with exercise, patient education, and behavioral therapies.
Anti-Seizure Agents (Anti-Convulsants)
Pregabalin is an anti-epileptic medicine. Also called anti-seizure drugs and anti-convulsants, these medicines affect the chemical messenger gamma aminobutyric acid (GABA), which helps prevent nerve cells from over-firing.
Research is indicating that pregabalin may improve sleep quality, fatigue symptoms, and fibromyalgia pain. The most common side effects include mild-to-moderate dizziness and sleepiness. Pregabalin can also impair motor function and cause problems with concentration and attention. Patients should talk to their doctor about whether pregabalin may affect their ability to drive.
Studies have shown that another anti-convulsant, gabapentin (Neurontin) relieves pain in some people with fibromyalgia and similar conditions. Patients have reported sleeping better and feeling less tired after taking this drug. However, gabapentin can cause side effects such as dizziness, sleepiness, and swelling.
Antidepressants
The main classes of antidepressants used for treating fibromyalgia are tricyclics, selective serotonin-reuptake inhibitors (SSRIs), and serotonin-norepinephrine reuptake inhibitors (SNRIs). Although these drugs are antidepressants, doctors prescribe them to improve sleep and relieve pain in non-depressed patients with fibromyalgia. The dosages used for managing fibromyalgia are generally lower than dosages prescribed for treating depression. If a patient has depression in addition to fibromyalgia, higher doses may be required.
Tricyclics. Tricyclic antidepressants were the first drugs to be well-studied for fibromyalgia. They may be more effective than SSRIs and SNRIs for fibromyalgia symptoms, although all three drug classes seem to show some effectiveness. Tricyclics cause drowsiness and can be helpful for improving sleep. Research finds that they are also effective for reducing pain, and improving depressed mood and quality of life. The tricyclic drug most commonly used for fibromyalgia is amitriptyline (Elavil, Endep), which produces modest improvements in pain and sleep but can lose effectiveness over time. Other tricyclics include nortriptyline (Pamelor, Aventyl), desipramine (Norpramin), doxepin (Sinequan), imipramine (Tofranil), and amoxapine (Asendin).
Generally, only small doses of tricyclic antidepressants are needed to relieve fibromyalgia. Therefore, although tricyclics have several side effects, these side effects may be less frequent in fibromyalgia patients than in people who are taking tricyclics for depression. The side effects most often reported include:
- Blurred vision
- Difficulty urinating
- Dizziness
- Drowsiness
- Dry mouth
- Heart rhythm disturbances
- Sexual dysfunction
- Weight gain
As with all medications, tricyclic antidepressants must be taken as directed. An overdose can be life threatening.
Unfortunately, not all patients respond to tricyclics, and the effects wear off in some patients, sometimes after only a month.
Selective Serotonin-Reuptake Inhibitors. Selective serotonin-reuptake inhibitors (SSRIs) increase serotonin levels in the brain, which may have specific benefits for fibromyalgia patients. Commonly prescribed SSRIs include fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), and fluvoxamine (Luvox). Studies suggest they may improve sleep, fatigue, and well-being in many patients. Studies are mixed on whether they improve pain. SSRIs should be taken in the morning, since they may cause insomnia. Common side effects are agitation, nausea, and sexual dysfunction, including a delay or loss of orgasm and low sex drive.
Serotonin-Norepinephrine Reuptake Inhibitors. Serotonin-norepinephrine reuptake inhibitors (SNRIs) are also known as dual inhibitors because they act directly on two chemical messengers in the brain -- norepinephrine and serotonin. These drugs appear to have more consistent benefits for fibromyalgia pain than SSRIs. They also tend to have fewer side effects than the tricyclics and are well tolerated.
SNRIs include:
- Duloxetine (Cymbalta) has been approved by the FDA for treating fibromyalgia. In studies, it reduced fibromyalgia pain by more than 30%. The most common side effects with this medication are nausea, dry mouth, constipation, decreased appetite, sleepiness, increased sweating, and agitation. Duloxetine may also increase the risk of hemorrhage in patients taking NSAIDs, aspirin, or blood thinners.
- Milnacipran (Savella) can significantly improve pain and physical function in fibromyalgia patients. Milnacipran is not approved for use in children. The label includes a boxed warning that it may increase the risk of suicidal thoughts and behaviors in children and adolescents. It is also not appropriate for patients who are taking monoamine oxidase inhibitors, and for those with uncontrolled narrow-angle glaucoma.
- Venlafaxine (Effexor) is similar to fluoxetine (Prozac) in effectiveness and tolerability. As with SSRIs, and unlike other newer antidepressants, venlafaxine impairs sexual function. Although clinical trials have shown that the drug is safe and effective in most people, there have been reports of changes in blood pressure. There have also been reports of problems with the electrical system of the heart in people taking this drug. These side effects may cause serious problems in elderly patients. Some patients also report severe withdrawal symptoms, including dizziness and nausea.
Muscle Relaxants
Cyclobenzaprine (Flexeril) relaxes muscle spasms in specific locations without affecting overall muscle function. It helps relieve fibromyalgia symptoms. Cyclobenzaprine is related to the tricyclic antidepressants and has similar side effects, including drowsiness, dry mouth, and dizziness.
Sleep Medications
Zolpidem (Ambien) or other newer sleep medications such as zaleplon (Sonata) and eszopiclone (Lunesta) may improve sleep in patients with insomnia.
Pain Relievers
Pain relief is of major concern for patients with fibromyalgia. Pain relievers for fibromyalgia include:
- Tramadol (Ultram), used alone or in combination with acetaminophen (Tylenol), is commonly prescribed for relief of fibromyalgia pain. Its most common side effects are drowsiness, dizziness, constipation, and nausea. Tramadol should not be used with tricyclic antidepressants. Patients may become dependent on this drug, and potentially abuse it.
- For relief of mild pain, acetaminophen is most often recommended. Anti-inflammatory drugs, which are commonly used for arthritic conditions, are less useful for the pain of fibromyalgia, because the pain is not caused by muscle or joint inflammation. Anti-inflammatory drugs include corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen (Advil). New guidelines from the American Geriatrics Society do not recommend the use of NSAIDs for older adults with chronic pain because the cardiovascular and gastrointestinal risks outweigh the benefits of using these drugs.
- Capsaicin (Zostrix) is an ointment prepared from the active ingredient in hot chili peppers. Capsaicin is helpful for relieving pain in other disorders. It may also have some value for fibromyalgia patients.
- Opioids or narcotics such as oxycodone (Roxicodone) or morphine sulfate (Duramorph) may be used occasionally by certain patients with moderate-to-severe pain, or those who have significant problems performing everyday tasks. These patients should use narcotics only if they cannot find relief with other, less potent treatments. Patients who are taking opioids should be evaluated periodically for pain relief, side effects, and signs of dependence.
- Pramipexole, a drug used to treat Parkinson's disease and RLS, may help relieve pain and fatigue in people with fibromyalgia. Pramipexole stimulates the production of dopamine, a chemical messenger in the brain.
- The atypical antipsychotic drug olanzapine (Zyprexa) may be a beneficial add-on therapy for patients with fibromyalgia. However, although olanzapine and other antipsychotics have been proven effective for some chronic pain conditions, they can cause unpleasant and potentially serious side effects.
Other Investigative Drugs
Nabilone. A synthetic drug derived from marijuana may be another effective addition to fibromyalgia treatment, according to early studies. In one study, nabilone (Cesamet), which is also used to treat severe nausea and vomiting in chemotherapy patients, significantly relieved fibromyalgia pain compared to placebo. There are some challenges to using nabilone for fibromyalgia, however. First, it is a controlled substance that can become addictive, and researchers say it is so expensive that it would be cost-prohibitive to use for a chronic disease such as fibromyalgia.
Resources
- www.rheumatology.org -- American College of Rheumatology
- www.niams.nih.gov -- National Institute of Arthritis and Musculoskeletal and Skin Diseases
- www.arthritis.org -- Arthritis Foundation
- www.fmaware.org -- National Fibromyalgia Foundation
- www.fmnetnews.com -- Fibromyalgia Network
- www.aapainmanage.org -- American Academy of Pain Management
- www.ampainsoc.org -- American Pain Society
- www.medicalacupuncture.org -- American Association of Medical Acupuncture
- www.asch.net -- American Society of Clinical Hypnosis
- www.clinicaltrials.gov -- Find a clinical trial
References
American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pain Med. 2009;10(6):1062-1083.
Arnold LM, Clauw DJ, McCarberg BH, and FibroCollaborative. Improving the recognition and diagnosis of fibromyalgia. Mayo Clin Proc. 2011;86(5):457-464.
Bennett RM. Clinical manifestations and diagnosis of fibromyalgia. Rheum Dis Clin North Am. 2009;35(2):215-232.
Buskila D. Pediatric fibromyalgia. Rheum Dis Clin North Am. 2009;35(2):253-261.
Clauw DJ. Fibromyalgia: An overview. Am J Med. 2009;122(12):S3-S13.
Eccleston C, Palermo TM, Williams AC, Lewandowski A, Morley S. Psychological therapies for the management of chronic and recurrent pain in children. Cochrane Database Syst Rev. 2009 Apr 15 (2):CD003968.
Fontaine KR. Effects of lifestyle physical activity on perceived symptoms and physical function in adults with fibromyalgia: results of a randomized trial. Arthritis Res Ther. 2010;12(2):R55.
Hassett AL, Gevirtz RN. Nonpharmacologic treatment for fibromyalgia: Patient education, cognitive-behavioral therapy, relaxation techniques, and complementary and alternative medicine. Rhem Dis Clin North Am. 2009;35(2):393-407.
Hauser W, Bernardy K, Uceyler N, Sommer C. Treatment of fibromyalgia syndrome with antidepressants. JAMA. 2009;301(2):198-209.
McBeth J, Prescott G, Scotland G, Lovell K, Keeley P, Hannaford P, et al. Cognitive behavior therapy, exercise, or both for treating chronic widespread pain. Arch Intern Med. 2011 Nov 14. [Epub ahead of print]
Mease PJ. Further strategies for treating fibromyalgia: The role of serotonin and norepinephrine reuptake inhibitors. Am J Med. 2009;122(12 Suppl):S44-S55.
Mease PJ. The efficacy and safety of milnacipran for treatment of fibromyalgia. A randomized, double-blind, placebo-controlled trial. J Rheumatol. 2009;36(2):398-409.
Moore RA, Straube S, Wiffen PJ, Derry S, McQuay HJ. Pregabalin for acute and chronic pain in adults. Cochrane Database Syst Rev. 2009;6(3):CD007076.
Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2011 Mar 16;(3):CD007938.
Paras ML, Murad MH, Chen LP, Goranson EN, Sattler AL, Colbenson KM, et al. Sexual abuse and lifetime diagnosis of somatic disorders: a systematic review and meta-analysis. JAMA. 2009;302(5):550-561.
Wang C. A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363(8):743-754.
Williams DA, Schilling S. Advances in the assessment of fibromyalgia. Rheum Dis Clin North Am. 2009;35(2):339-357.
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg Dl, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010;62(5):600-610.
|
Review Date:
2/7/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |



