Colon and rectal cancers
Highlights
Colorectal Cancer Screening Guidelines
A number of major organizations, including The American Cancer Society, The U.S. Preventive Services Task Force, the American College of Physicians, and The American College of Gastroenterology, have created guidelines related to screening for colorectal cancer. While there are some differences between these guidelines, in general they recommend that adults ages 50 - 75 who are at average risk for colorectal cancer should be screened with one of these methods:
- Colonoscopy every 10 years
- Flexible sigmoidoscopy every 5 - 10 years
- Double-contrast barium enema (DCBE) every 5 years
- CT colonography (CTC), also called virtual colonoscopy, every 5 years
Stool test options for screening include:
- Guiaiac-based fecal occult blood test (FOBT) every year
- Fecal immunochemical test (FIT) every year
- Stool DNA test (sDNA) every 3 years
Drug Approval
In 2012, two new biologic drugs were approved for treatment of advanced colorectal cancer:
- Ziv-aflibercept (Zaltrap) works by blocking the development of blood vessels that feed tumor growth. It is given by intravenous injection.
- Regorafenib (Stivarga) is the first biologic drug for colorectal cancer that comes in pill form. It blocks several different enzymes that are involved with cancer cell growth.
Aspirin for Colorectal Cancer Prevention
Several recent studies have called attention to the possible use of aspirin to prevent colorectal cancer and to reduce the risk of recurrent cancer in patients who have been treated for the disease. In particular, aspirin may be helpful for people at risk for certain hereditary forms of colorectal cancer. However, long-term use of aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) can cause stomach bleeding and other health problems. At this time, the American Cancer Society, the U.S. Preventive Services Task Force, and other professional organizations do not recommend aspirin for colorectal cancer prevention in people at average risk for the disease.
Introduction
Cancers of the colon and rectum, often collectively referred to as colorectal cancer, are life-threatening tumors that develop in the large intestine.
More than 80% of colorectal tumors develop from adenomatous polyps. These gland-like growths develop on the mucous membrane that lines the large intestine. They are usually either:
- Tubular polyps, which protrude mushroom-like
- Villous adenomas, which are flat and spreading and are more apt to become malignant (cancerous)
Polyps are very common, and most of them are benign. Their numbers increase with age. Polyps are found in about 25% of people by age 50, and 50% of people by age 75. Fewer than 1% of polyps under 1 centimeter (slightly less than half an inch) become cancerous. About 10% of larger polyps become cancerous within 10 years, and about 25% of these larger polyps become cancerous after 20 years.
The Gastrointestinal Tract
Digestion takes place in the gastrointestinal (GI) tract, basically a long tube that extends from the mouth to the anus. It is a complex organ system that first carries food from the mouth down the esophagus to the stomach. Food then travels through the small and large intestines before being excreted through the rectum and out the anus.
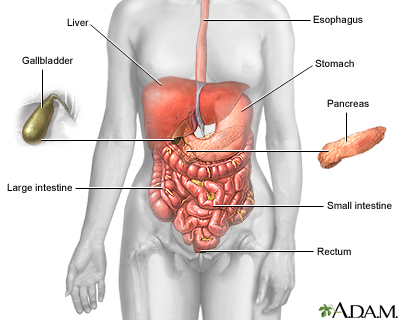
Esophagus
The esophagus is a narrow muscular tube, about 9 1/2 inches long, that begins below the tongue and ends at the stomach.
Stomach
In the stomach, acids and stomach motion break food down into particles small enough so that the small intestine can absorb nutrients.
Small Intestine
The small intestine, despite its name, is the longest part of the gastrointestinal tract, extending for about 20 feet. Food passes from the stomach through its three parts: first the duodenum, then the jejunum, and finally the ileum. Most of the digestive process occurs in the small intestine.
Large Intestine (Colon)
Undigested material, such as plant fiber, is passed next to the large intestine, or colon, mostly in liquid form. The colon is wider than the small intestine but only about 6 feet long. The colon absorbs excess water and salts into the blood. The remaining waste matter is converted to feces through bacterial action. The colon is a continuous structure but it is characterized as having several components.
Cecum and Appendix. The cecum is the first part of the colon and it gives rise to the appendix. These structures are located in the lower-right quadrant of the abdomen. The colon continues onward in several sections:
- The first section, the ascending colon, extends upward from the cecum on the right side of the abdomen.
- The second section, the transverse colon, crosses the upper abdomen to the left side.
- The third section extends downward on the left side of the abdomen toward the pelvis and is called the descending colon.
- The final section is the sigmoid colon.
Rectum and Anus. Feces are stored in the descending and sigmoid colon until they are passed through the rectum and anus. The rectum extends through the pelvis from the end of the sigmoid colon to the anus.
Causes
In most cases of colon or rectal cancers, the cause or causes are unknown. Defects in genes that normally protect against cancer play the major role in causing polyp cells to change and become cancerous. Sometimes these cancerous changes are caused by inherited genetic defects, and such patients usually have family histories of colorectal cancer. Most of the genetic mutations involved in colon cancers, however, appear to arise spontaneously (no strong family history) rather than being inherited. In such cases, environmental or other factors may trigger genetic changes in the intestine that lead to cancer.
Risk Factors and Prevention
Colorectal cancer is the third most common cancer in the United States. About 72% of colorectal cancers occur in the colon and 28% in the rectum.
Rates of colorectal cancer have been decreasing in the United States. This is due in part to more people getting regular screenings for colorectal cancer, and fewer people engaging in risk factors such as smoking.
Age
Colorectal cancer risk increases with age. More than 90% of these cancers occur in people over age 50.
Gender
Men have a slightly higher risk than women for developing colorectal cancer.
Race and Ethnicity
African-Americans have the highest risk of being diagnosed with, and dying from, colorectal cancer. Among Caucasians, Jews of Eastern European (Ashkenazi) descent have a higher rate of colorectal cancer. Asian Americans/Pacific Islanders, Hispanics/Latinos, and American Indians/Alaska Natives have a lower risk than Caucasians.
Family History of Colorectal Cancer
About 20 - 25% of colorectal cancers occur among people with a family history of the disease. People who have more than one first-degree relative (sibling or parent) with the disease are especially at high risk. The risk is even higher if the relative was diagnosed with colorectal cancer before the age of 60.
A small percentage of patients with colorectal cancer have an inherited genetic abnormality that causes the disease. Syndromes associated with genetic mutations include familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer.
- Familial Adenomatous Polyposis (FAP). Familial adenomatous polyposis is caused by mutations in a gene called the adenomatous polyposis coli (APC) gene, which normally helps suppress tumor growth. In its defective form, it accelerates cell growth leading to polyps. The APC mutation can be inherited from either parent. People with FAP develop hundreds to thousands of polyps to in the colon. If FAP is left untreated, virtually everyone who inherits this condition develops cancer by age 45. Polyps usually first appear when people are in their mid-teens. FAP also increases the risks for other types of cancers including stomach, thyroid, pancreatic, liver, and small intestine cancers.
- Hereditary Nonpolyposis Colorectal Cancer (HNPCC). Hereditary nonpolyposis colorectal cancer (HNPCC) is also known as Lynch syndrome. About 50 - 80% of people who inherit the abnormal gene develop colon cancer by age 45. HNPCC is caused by mutations in several genes. People with HNPCC are prone to other cancers, including uterine and ovarian cancers, as well as cancers of the small intestine, liver, urinary tract, and central nervous system.
Lifestyle Factors
Colon cancer is more common in developed nations than less developed countries. “Western” lifestyle factors are most likely the reason. Diets high in red and processed meats, lack of physical activity, excess weight, and smoking are all associated with increased risk for colorectal cancer.
Dietary Factors. A diet high in red and processed meats increases the risk for colorectal cancer. Diets high in fruits and vegetables may help reduce risk. The evidence is mixed on whether high intake of dietary fiber is protective. It is also not clear whether there is an association between colorectal cancer risk and deficiencies of the B vitamin folic acid. In any case, neither folic acid nor fiber supplements appear to lower the risk for colorectal cancer. The best sources for dietary fiber and vitamins are fruits, vegetables, nuts, and whole grains.
Alcohol and Smoking. Excessive alcohol use and long-term smoking are associated with increased risk for colorectal cancer. .
Obesity. Obesity is associated with an increased risk for colorectal cancer, especially for men.
Physical Inactivity. A sedentary lifestyle increases the risk of developing colorectal cancer. Regular exercise may help reduce risk.
Medical Conditions That Increase Colorectal Cancer Risk
Adenomatous Polyps. People who have had adenomatous polyps (adenomas) have an increased risk of developing colorectal cancer. When these polyps are detected during a colonoscopy or sigmoidoscopy they can be removed before they turn cancerous.
Inflammatory Bowel Disease. Inflammatory bowel diseases include Crohn's disease and ulcerative colitis. The long-term inflammation caused by these chronic disorders can increase the risk for colorectal cancer. Inflammatory bowel disease (IBD) is different from irritable bowel syndrome (IBS), which does not increase colorectal cancer risk.
Diabetes. Many studies have identified an association between type 2 diabetes and colon cancer. Both diseases share common risk factors of obesity and physical inactivity, but diabetes itself is a risk factor for colorectal cancer.
Preventive Factors
Colorectal cancer screenings are a very important preventive measure. Healthy lifestyle measures are also extremely important. For people with certain type of colorectal cancer risk factors, preventive medications may be helpful.
Lifestyle Changes and Prevention. The best way to prevent colorectal cancer is to engage in a healthy lifestyle:
- Exercise regularly
- Eat a healthy diet low in meat and high in fruits, vegetables, and whole grains
- Do not smoke
- Do not drink alcohol in excess.
Medications and Prevention. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used pain relievers that include aspirin, ibuprofen (Advil, Motrin, generic), naproxen (Aleve, generic), and the COX-2 inhibitor celecoxib (Celebrex).
- Recent studies suggest that daily low-dose aspirin may help prevent colorectal cancer in people who are at high-risk for genetic forms of the disease, such as Lynch syndrome.
- There is also some evidence that aspirin therapy may help improve odds of survival after a diagnosis of colorectal cancer (secondary prevention).
- However, long-term use of aspirin and other NSAIDs carries serious risks for stomach bleeding. The American Cancer Society and the U.S. Preventive Services Task Force (USPSTF) do not recommend the routine use of aspirin, other NSAIDs, or other types of medications to prevent colorectal cancer in people at average risk for this disease.
Symptoms
It is common to have colon or rectal cancer without symptoms. Many patients are free of symptoms until their tumors are quite advanced.
Symptoms associated with colorectal cancer may also be caused by other conditions. These symptoms include:
- Changes in bowel movements, such as diarrhea or constipation, or change in consistency or size of stools
- Feeling that the bowel has not emptied completely after a bowel movement
- Abdominal discomfort such as gas, bloating, and cramps
- Rectal bleeding or blood in stool
- Pain when having a bowel movement
- Unexplained weight loss
- Unexplained iron-deficiency anemia (low red blood cell count)
- Weakness and fatigue
Diagnosis and Screening
Colon and rectal cancers can be detected early using the screening tests discussed below. These tests can find precancerous polyps and colorectal cancers at stages early enough for complete removal and cure.
Colorectal Cancer Screening Guidelines
The American Cancer Society (ACS), the U.S. Preventive Services Task Force (USPSTF), the American College of Physicians, and the American College of Gastroenterology (ACG) all have made similar, although not identical, recommendations concerning screening for colorectal cancer. Discuss with your doctor whether you are at average- or high-risk for colorectal cancer, and which screening test and schedule is most appropriate for you. (See descriptions of screening tests below for more information about the individual tests.)
Screening for Adults with Average Risk for Colorectal Cancer.
General age recommendations for colorectal cancer screening are:
- Screening should begin at age 50 years and continue until age 75.
- Screening is not routinely recommended for adults age 75 and older. However, the decision to screen needs to be made on an individual basis.
Several options and schedules for screening are recommended. The choices include:
- Colonoscopy every 10 years
- Flexible sigmoidoscopy every 5 - 10 years
- Double-contrast barium enema (DCBE) every 5 years
- CT colonography (CTC), also called virtual colonoscopy, every 5 years
Stool tests are another option:
- Guaiac-based fecal occult blood test (FOBT) every year
- Fecal immunochemical test (FIT) every year
- Stool DNA test (sDNA) every 3 years
- If a stool test shows an abnormal result, a colonoscopy is required
Screening for Adults at High-Risk for Colorectal Cancer. Patients at high risk for colorectal cancer should choose colonoscopy for screening. The most important risk factors that may prompt screening before age 50 or frequent screenings are:
- A known family history of inherited colorectal cancer syndromes such as familial adenomatous polyposis (FAP) or hereditary nonpolyposis colorectal cancer (HNPCC)
- A strong family history of colorectal cancer or polyps, especially in first-degree relatives (parent, sibling, or child) who developed these conditions younger than age 60
- A personal history of colorectal cancer or polyps
- A personal history of chronic inflammatory bowel disease. [For specific screening recommendations for patients with inflammatory bowel disease, see In-Depth Reports #103: Crohn's disease and #69: Ulcerative colitis.]
Patients in these high-risk groups who have changes that are identified as precancerous during colonoscopy will likely have their doctors discuss with them the possibility of a prophylactic or preventive colectomy (removal of the colon).
Description of Screening Tests
Colonoscopy. Colonoscopy allows a doctor to view the entire length of the large intestine using a colonoscope, which is inserted into the rectum and snaked through the intestine. A colonoscope is a long, flexible tube that has a video camera one end. The doctor views images from the colonoscope on a display monitor. The test takes about 30 minutes to perform. If polyps are found, the doctor will remove them. The patient is given a sedative prior to the test, which produces a comfortable “twilight” sleep.
In order for the doctor to perform a successful colonoscopy, the colon and rectum must be completely empty. Your doctor will give you complete instructions for how to prepare during the days preceding the tests, and specific foods and liquids to avoid eating and drinking. The day before the test you will be given laxative solution to clean out the colon. Many people find this cleansing more unpleasant than the colonoscopy itself.
Colonoscopy is generally a safe procedure. In very rare cases, complications such as bowel perforation can occur.
Flexible Sigmoidoscopy. Sigmoidoscopy is similar to colonoscopy but only examines the rectum and the lower two feet of the colon. (In contrast, colonoscopy allows the doctor to view the entire colon.) The procedure takes about 10 - 20 minutes, and sedation is optional. Preparation procedures are less demanding than those for colonoscopy.
Double-Contrast Barium Enema (DCBE). The double-contrast barium enema test uses an x-ray to image the entire large intestine. The test takes about 30 - 45 minutes, and sedation is not required. Preparations are similar to those for colonoscopy and sigmoidoscopy. For the test, barium sulfate is inserted into the rectum using a small, flexible tube. The colon is then pumped with air to help the barium spread through the colon. If polyps are detected in the x-ray, your doctor may recommend you have a colonoscopy for further investigation and removal.
Virtual Colonoscopy. Virtual colonoscopy, also called CT colonoscopy, uses x-rays delivered by computed tomography (CT) scan to take three-dimensional images of the colon. The test takes only 10 minutes to perform, and does not require sedation. (It does require the same preparations as standard colonoscopy to clean out the colon and bowel.) Air is pumped into the rectum through a small flexible tube. The patient is then slid into a CT scanner, which takes rapid images. Some recent studies indicate that CT colonoscopy has a high accuracy rate in detecting adenomas and cancers. if polyps are detected, a standard colonoscopy is required.
Fecal Occult Blood Test (FOBT). A fecal occult blood test is a take-home test that uses stool samples to detect hidden (occult) blood in feces. It may detect small amounts of blood in your stool from polyps or a tumor, even when your stools appear normal. Your doctor will give you a kit with instructions on how to take stool samples and prepare them for the kit. Your doctor will also inform you about what medications and foods need to be avoided in the days prior to the test. The test kit and samples are sent to a laboratory and results usually come back in a short time. If blood is found in the stool samples, you will need to have a colonoscopy.
Fecal Immunochemical Test (FIT). The fecal immunochemical test is a newer type of take-home test for hidden (occult) blood. The test is similar to the fecal occult blood test, but patients do not need to follow medication or dietary restrictions. As with the FOBT, a colonoscopy is recommended if blood is found in the stool.
Stool DNA Test. Like the FIT and the FOBT, the stool DNA test is conducted at home and uses fecal samples. Instead of testing for the presence of blood, this test looks for abnormalities in genetic material that come from cancer or polyp cells. These genetic changes are found in genes such as APC, K-ras, and p53. If DNA mutations are found, a colonoscopy is needed. The stool DNA test is new and not yet widely available. Some insurance carriers may not cover its cost.
Diagnosis of Colorectal Cancer
A doctor makes a diagnosis of colorectal cancer based on results of several types of tests. These tests include:
Biopsy. During a colonoscopy, the doctor can remove a tissue sample, which is sent to a laboratory for testing. A biopsy is the only way to definitively diagnose colorectal cancer.
Blood Tests. Blood tests are used to evaluate the red blood cell count and check for anemia. The presence of anemia without any other obvious cause being present will usually require further evaluation of the gastrointestinal tract for a possible cancer. Blood tests are also used to check for specific tumor markers, substances that are released into the blood from cancer cells. Tumor markers include carcinoembryonic antigen (CEA) and CA 19-9. These tests may help your physician follow you for recurrences of colon cancer after treatment. By themselves, they cannot diagnose cancer and are not used as a screening test
Imaging Tests. Various types of imaging tests can help detect the presence of cancer or find out how far the cancer has spread. These tests include ultrasound, chest x-ray, magnetic resonance imaging (MRI) scan, positron emission tomography (PET) scan, and computed tomography (CT) scan.
Treatment
A diagnosis of cancer will lead to staging and other tests to help determine the outlook and the appropriate treatments. Treatment for colorectal cancer includes surgery, chemotherapy, and radiation. These treatment methods may be combined.
- Surgery is used for early-stage colorectal cancer. Usually, the tumor is removed along with part of the colon and nearby lymph nodes.
- Chemotherapy may be given after surgery to kill any remaining cancer cells. It may also be given along with radiation before surgery to reduce tumor size.
- Radiation therapy is not usually used in early-stage colon cancer, but is commonly used to treat early-stage rectal cancer. It is often combined with chemotherapy.
- Clinical trials are available for individual stages of colorectal cancer.
Colorectal Cancer Stages and Treatment Options
There are several methods for staging colorectal cancer. The older system, known as Dukes', categorizes four basic stages: A, B, C, and D. The newer TMN system evaluates the tumor (T), lymph node (N), and how far the cancer has spread or metastasized (M). The results of TMN are combined to determine the stage of the cancer.
Colorectal cancer stages and treatment options are: Stage 0 (Carcinoma in situ).
- In stage 0, cancer cells are fully contained in the innermost lining (mucosa) of the colon or rectum, and have not yet invaded the wall of the colon
- Treatment for stage 0 cancer usually involves surgical removal of the polyp (polypectomy) during colonoscopy.
Stage I
- In stage I, the cancer has spread through the mucosa of the colon wall into middle layers of tissue.
- Treatment for stage I involves resection of the tumor. The tumor may be removed along with part of the colon (colectomy).
Stage II
- In stage IIA, the cancer has spread beyond the middle layers to the outer tissues of the colon or rectum. In stage IIB, the cancer has penetrated through the colon or rectum wall into nearby tissue or organs.
- Treatment for stage II cancer involves surgical resection. Chemotherapy after surgery (adjuvant chemotherapy) plus radiation is considered standard treatment for stage II rectal cancer, but is under debate for stage II colon cancer.
Stage III
- In stage III, lymph nodes are involved but not distant sites. Stage IIIA and IIIB cancer has spread to as many as three lymph nodes. Stage IIIC cancer involves four or more lymph nodes.
- Treatment for stage III colon cancer involves surgery and adjuvant chemotherapy with the FOLFOX regimen (5-FU, leucovorin, oxaliplatin). For patients with stage III rectal cancer, treatment includes chemotherapy and radiation, either before or following surgery.
Stage IV
- Stage IV is metastasized cancer. The cancer has spread to nearby lymph nodes and to other organs of the body such as the liver or lungs.
- Treatment for stage IV cancer may sometimes include surgery. When cancer has spread, surgery to remove or bypass obstructions in the intestine may be performed. In these circumstances, surgery is considered palliative in that it may improve symptoms but will not lead to cure. In some cases, surgery may also be performed to remove tumors in areas that the cancer has spread, such as the liver, ovaries, or lung.
- Chemotherapy is standard treatment for metastasized cancer. In advanced colorectal cancer, chemotherapy is either given directly into the arteries of the liver when it is involved or intravenously (through a vein). There are many different chemotherapy regimens. Most use fluorouracil (5-FU) in combination with other cancer-fighting drugs. “Targeted therapy” with a biologic drug may also be an option for some patients. Radiation therapy may be used in place of chemotherapy or in combination with it. Radiation is often used as palliative treatment to help ease symptoms and reduce pain.
Prognosis
Colorectal cancer is among the most curable of cancers when it is caught in its early stages. The term "5-year survival" means that patients have lived at least 5 years since diagnosis. The 5-year survival rate for colon cancer diagnosed and treated at stage I is 74%. The rates fall to 37 - 67% for stage II, 28 - 73% for stage III, and 6% for stage IV. However, there are other factors, including the appearance of cancer cells under the microscope, which can contribute to a patient's prognosis.
Follow-Up Monitoring
Doctors recommend follow-up testing to detect recurring cancer after the completion of treatment. General guidelines include:
Physical Examination. Most colorectal cancer recurrences happen within 3 years after surgery. Patients should see their doctors for a physical examination every 3 - 6 months for the first 2 years following surgery, every 6 months through the fifth year, and at the doctor's and patient's discretion during subsequent years.
Colonoscopy. Patients should have a colonoscopy 1 year after surgery. If the results are normal, patients should then receive a colonoscopy 3 years later and then every 5 years. Patients with abnormal results or who have hereditary types of cancer may need more frequent screenings.
A flexible sigmoidoscopy is recommended every 6 months for 5 years for patients with Stage II or III rectal cancer who did not receive radiation therapy.
Carcinoembryonic Antigen Levels. Carcinoembryonic antigen (CEA) levels should be measured every 3 - 6 months after surgery for 2 years in patients, and then every 6 months up to 5 years for patients with Stage II or III cancer. High CEA levels in the blood may indicate that the cancer has recurred or has spread to other parts of the body.
Imaging Tests. Patients at high risk for cancer recurrence should receive an annual computerized tomography (CT) scan of the chest, abdomen, and pelvis for the first 3 years after treatment. The CT scan can help determine if cancer has spread to the lungs or liver. Patients who have had rectal cancer, and did not have radiation therapy, should receive a pelvic CT scan. The scan is not recommended for most lower-risk patients with Stage I or II colorectal cancer. PET scans are not routinely recommended.
Other Tests. The American Society of Clinical Oncology does not recommend other follow-up blood tests such as complete blood count, liver function tests, and fecal occult blood tests. There appears to be no additional benefit for these tests.
Surgery
In the earliest stages of colorectal cancer (stage 0 and some stage I cases) polyps can be removed during a colonoscopy in a procedure called polypectomy. Early-stage superficial cancers that are not deep can also be removed through excision, where the cancer is cut out by inserting a tube into the rectum. Unlike colectomy, these procedures do not involve cutting through the abdominal wall.
Surgical removal of the tumor ("resection") along with any affected surrounding tissue is the standard initial treatment for potentially curable colorectal cancers (cancers that have not spread beyond the colon or lymph nodes). Drug and radiation therapy are often used for advanced cancers and are continuously being tested with surgery in different combinations and sequences.
Although choosing a qualified surgeon is critical, choosing a hospital experienced in procedures is also important. The more often colon cancer surgery is performed at a given hospital, the lower the mortality rate at that hospital is likely to be.
Colectomy
Unless cancer is very advanced, most tumors are removed by an operation known as colectomy:
- Colectomy involves removing the cancerous part of the colon and nearby lymph nodes.
- The surgeon then reconnects the intestine in a procedure called anastomosis.
- If the surgeon cannot reconnect the intestine, usually because of infection or obstruction, the surgeon will perform a colostomy. Colostomy is a surgical procedure that brings one end of the large intestine out through the abdominal wall. Stools moving through the intestine drain into a bag (ostomy pouch) attached to the abdomen. The need for colostomies is higher after surgery for rectal cancer. In most cases of colon cancer, colostomies are not needed. [See "Colostomy" below.]
- Stents, expandable metal tube-like devices, may be used as preparation before surgery to remove blockage and to keep the intestine open.
The Surgical Approach. The standard technique for a colectomy is open, invasive surgery. Laparoscopy, sometimes called “keyhole surgery,” is a newer less invasive method.
- Open surgery uses a wide incision to open the patient's abdomen. The surgeon then performs the procedures with standard surgical instruments. This is the usual method for performing colectomy.
- Laparoscopy uses a few small incisions through which the surgeon passes a fiber optic tube (laparoscope) containing a small camera or tiny instruments. It is generally used for early colon cancer (for tumors less than 2 centimeters or for well-defined tumors less than 3 centimeters).
Colostomy
A colostomy is performed in order to bypass or remove the lower colon and rectum. The procedure generally involves creating a passage, called a stoma, through the abdominal wall that is connected to the colon. The feces pass through this passage and are eliminated. Patients must learn how to care for the stoma and keep the area sanitary.
A colostomy usually will have one opening (single-barreled), or there may be two loops opening through the skin (double-barreled).
Usually the colostomy is temporary and can be reversed by a second operation after about 3 - 6 months. If the rectum and sphincter muscles in the rectum need to be removed, the colostomy is permanent. Permanent colostomies are more common when the cancerous regions are within 2 - 3 centimeters of the anus. Fortunately, surgical advances and knowledge of the extent of safe margins are reducing the need for permanent colostomies.
Managing Permanent Colostomies. In cases where the colostomy is permanent, the patient must wear a colostomy pouch, which sticks to the skin using a special glue.
For best results, the pouch should be emptied when about one-third full. It should be replaced 1 - 2 times a week, depending on signs of leakage (itching or burning of the skin near the stoma). The pouches are odor proof.
Surgical Treatments for Rectal Cancer
Surgical treatments for cancer in the rectum are complex since they involve muscles and tissue that are critical for urinary and sexual function.
Local Excision or Polypectomy for Early Stages. In order to preserve the function of the anal sphincter and prevent the need for colostomy, Stage I and Stage II tumors may be removed by local excision, sometimes followed by chemotherapy and radiation. In this procedure, the tumor is cut out without removal of a major section of rectum. In some cases cancer recurs, but a second operation may be possible.
Radical Resection. In about a third of cases of rectal cancer, the cancer occurs in the lower part of the rectum, spreading beyond the rectal wall. These patients need a radical resection, in which surrounding structures, including the sphincter muscles that control bowel movements, must often be removed.
Total Mesorectal Excision. Total mesorectal excision (TME) involves dissection and removal of the entire cancerous area of the rectum along with surrounding fatty regions where the lymph nodes are located (the mesorectum). When successful, TME preserves the sphincter muscle, reducing the need for a permanent colostomy.
Managing Side Effects
Side effects of colon surgery may include:
- Sexual dysfunction. In general, colostomy does not usually affect sexual function. However, wide rectal surgery can cause short- or long-term sexual dysfunction. PDE5 inhibitor drugs such as sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis) may help men who experience this after surgery.
- Irregular bowel movements.
- Gas and flatulence. Pouching filters are available to reduce gas. Certain foods produce more gas than others -- usually within 6 - 8 hours after ingestion -- for colostomy patients. They include beans, oat bran, most fruit, and certain vegetables (cabbage, cauliflower, Brussels sprouts, broccoli, and asparagus). To prevent swallowing air, patients should avoid sipping through straws, chewing gum, and chewing with their mouths open.
- Diarrhea.
- Bladder complications.
- Sense of urinary urgency.
- Fecal incontinence. Patients with rectal surgery have a higher risk for bowel dysfunction than those who had a colostomy.
- Complications in or around the stoma. These can occur early after surgery to many years after the procedure. They include skin infection or breakdown, hernias, narrowing of the stoma, bleeding, and collapse.
There are no dietary restrictions, although many patients avoid foods that can produce gas. Everyone should drink plenty of fluids and get sufficient fiber.
The potential side effects of sexual and bowel dysfunction following colorectal surgery can be very difficult, although many patients do very well and live normal productive lives. Patients who are depressed should discuss with a doctor all aspects of treatment that affect the quality of life, and consider seeking support groups.
Chemotherapy
Chemotherapy Drugs and Regimens
Seven drugs are currently approved for colorectal cancer chemotherapy:
- 5-fluorouracil (5-FU, Adrucil), which is often given in combination with leucovorin (Wellcovorin). Leucovorin helps boost the effectiveness of 5-FU.
- Capecitabine (Xeloda)
- Oxaliplatin (Eloxatin)
- Irinotecan (Camptosar)
- Bevacizumab (Avastin)
- Cetuximab (Erbitux)
- Panitumumab (Vectibix)
Capecitabine is a pill form of 5-FU. The other drugs are administered intravenously. Many of these drugs are given in combination with each other. Common chemotherapy combination regimens include:
- 5-FU / LV (5-FU and leucovorin)
- FOLFOX (5-FU with leucovorin and oxaliplatin)
- FOLFORI (5-FU with leucovorin and irinotecan)
- FOLFIRI (5-FU with folinic acid and irinotecan)
- IFL (Irinotecan, 5-FU, leucovorin)
- XELOX (Capecitabine and oxaliplatin)
Side effects occur with all chemotherapeutic drugs. They are more severe with higher doses and increase over the course of treatment. Because cancer cells grow and divide rapidly, chemotherapy drugs work by killing fast-growing cells. This means that healthy cells that multiply quickly can also be affected. The fast-growing normal cells most likely to be affected are blood cells forming in the bone marrow, and cells in the digestive tract, reproductive system, and hair follicles.
Nausea and vomiting are very common side effects, but drugs such as ondansetron (Zofran) can help provide relief. In general, side effects are nearly always temporary, and medications can help manage them.
Specific Chemotherapy Drugs
5-Fluorouracil (5-FU) with Leucovorin. Adjuvant (following surgery) chemotherapy using 5-fluorouracil, either alone or with leucovorin (5-FU/LV), is the standard treatment for patients with high-risk colon cancer (Stage III or select patients with Stage II tumors). Patients are given a series of cycles that usually continue for at least 6 months. Leucovorin, is related to folinic acid, a form of the B vitamin folic acid, and helps increase 5-FU’s effectiveness. If leucovorin is not available, a related drug, levoleucovorin (Fusilev), may be given as an alternative. Levoleucovorin in combination with 5-FU is approved for palliative (symptom) treatment of advanced metastatic cancer.
There are many different ways of giving 5-FU, including intravenously over several hours once a week, intravenously daily for 5 consecutive days every month, or as continuous infusion with a portable pump. The most common side effects include nausea and vomiting, diarrhea, loss of appetite, hair loss, swelling of hands and feet, rashes, and mouth sores.
Irinotecan. Irinotecan (Camptosar) blocks an enzyme essential for cell division. Irinotecan can be given alone or in combination with 5-FU and leucovorin. This combination therapy (irinotecan plus 5-FU/LV) is also referred to as the "Salz regimen," or IFL. Diarrhea is a common side effect of irinotecan.
Capecitabine. Capecitabine (Xeloda), a pill form of 5-FU, is used as a treatment for stage III and stage IV (metastatic) colorectal cancer. It is the only pill approved for colorectal cancer. Oxaliplatin. Oxaliplatin (Eloxatin) is related to cisplatin, a widely used platinum-based chemotherapy drug. Oxaliplatin is used in combination with 5-FU and leucovorin. This triple combination therapy is called the FOLFOX regimen. Capecitabine may also be used in combination with bevacizumab as a treatment option for initial therapy of advanced or metastatic cancer.
Oxaliplatin. Oxaliplatin (Eloxatin) is related to cisplatin, a widely used platinum-based chemotherapy drug. Oxaliplatin is used in combination with 5-FU and leucovorin in the FOLFOX regimen. Oxaliplatin can cause pain and tingling sensations in the hands and feet (neuropathy) that is worsened by exposure to cold.
Biologic Drugs
Traditional chemotherapy drugs can be effective, but because they do not distinguish between healthy and cancerous cells their generalized toxicity can cause severe side effects. “Targeted therapies” work on a molecular level by blocking specific mechanisms associated with cancer cell growth and division.
Biologic drugs are used to treat metastatic colorectal cancer (advanced cancer that has spread from the colon or rectum to other parts of the body). In general, they prolong survival by a few months. These drugs include:
- Bevacizumab (Avastin) is approved as a first-line treatment for patients with metastatic colorectal cancer. It is used in combination with IFL (irinotecan, 5-FU, leucovorin). Bevacizumab is a anti-angiogenic drug that targets and inhibits vascular endothelial growth factor (VEGF), a protein that regulates angiogenesis (the development of new blood vessels that feed a tumor's blood supply). Bevacizumab is given by intravenous infusion.
- Ziv-Aflibercept (Zaltrap) is another anti-angiogenesis drug. It is used along with the FOLFIRI (5-FU, folinic acid, irinotecan) as a second-line treatment for patients who were not helped by FOLFOX or other oxaliplatin-based chemotherapy regimens. Ziv-aflibercept is administered by intravenous infusion.
- Cetuximab (Erbitux) targets epidermal growth factor receptor (EGFR), a protein that fuels cancer cell proliferation. It can be used either in combination with irinotecan or alone for patients who have not responded to irinotecan. It is given by intravenous infusion. Guidelines recommend that cetuximab, and panitumumab (see below), should be given only to patients with tumors that express the wild-type KRAS gene. Patients with metastatic cancer should have tumors tested for KRAS gene status.
- Panitumumab (Vectibix) is another biologic drug that targets EGFR. It is used as a single drug and is given by intravenous infusion.
- Regorafenib (Stivarga) is a multi-kinase inhibitor that blocks several enzymes involved with cancer cell growth. Unlike the other biologic drugs used for colorectal cancer treatment, regorafenib is a pill that is taken by mouth.
Radiation
Radiation therapy uses x-rays to kill cancer cells that might remain after an operation or to shrink large tumors before an operation so that they can be removed surgically. The object of radiation therapy is to damage the tumor as much as possible without harming surrounding tissues. Radiation may be administered in one of the following two ways:
- Externally from a source outside the body, such as a linear accelerator (external beam radiation)
- Internally through small radioactive pellets implanted directly into the tumor (brachytherapy)
Preoperative and Postoperative Radiation with Chemotherapy
The main use for radiation therapy in people with colon cancer is when the cancer has attached to an internal organ or the lining of the abdomen. When this occurs, the surgeon cannot be certain that all the cancer has been removed, and radiation therapy may be used to kill any cancer cells remaining after surgery. Radiation therapy is seldom used to treat metastatic colon cancer because of side effects, which limit the dose that can be used.
For rectal cancer, radiation therapy is usually given to help prevent the cancer from coming back in the pelvis where the tumor started. It may be given either before or after surgery, but recently doctors have begun to favor preoperative treatment, along with chemotherapy. If a rectal cancer's size or position make surgery difficult, radiation may be used before surgery to shrink the tumor. Radiation therapy can also be given to help control rectal cancers in people who are not healthy enough for surgery.
Radiation also may be used to ease (palliate) symptoms in people with advanced cancer causing intestinal blockage, bleeding, or pain.
Radiation treatment is often combined with chemotherapy. Chemotherapy helps make the radiation treatment more effective. Radiation therapy is more often used for rectal cancer but may also be used in some cases for colon cancer.
Radiation for Colon Cancer. Radiation for colon cancer is given after surgery (postoperative or adjuvant radiation) to destroy any remaining cancer cells. It is generally not used to treat metastatic colon cancer.
Radiation for Rectal Cancer. Adjuvant radiation is a common practice for patients with rectal cancer in Stages II and III. Radiation is used to help prevent cancer recurrence. In recent years, doctors have also begun administering chemotherapy and radiation before surgery for rectal cancer (neoadjuvant chemoradiation). The use of radiation before surgery can help shrink the size of the tumor. Pre-operative chemotherapy and radiation may also help preserve sphincter-muscle function and reduce the chance that a patient will need a colostomy.
Side Effects of Radiation Therapy
Side effects of radiation may include:
- Diarrhea
- Skin irritation around the anus
- Incontinence
- Bladder irritation
- Fatigue
- Sexual dysfunction in men and vaginal irritation in women
Resources
- www.cancer.org -- American Cancer Society
- www.cancer.gov -- National Cancer Institute
- www.asco.org -- American Society of Clinical Oncology
- www.cancer.net -- Cancer.Net
- www.nccn.org -- National Comprehensive Cancer Network
- www.fightcolorectalcancer.org -- Colorectal Cancer Coalition
- www.cancer.gov/clinicaltrials -- Find clinical trials
References
American Cancer Society. Colorectal Cancer Facts & Figures 2011-2013. Atlanta: American Cancer Society, 2011.
Aune D, Chan DS, Lau R, Vieira R, Greenwood DC, Kampman E, et al. Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2011 Nov 10;343:d6617. doi: 10.1136/bmj.d6617.
Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011 Jun 8;305(22):2335-42.
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008 Dec 17;300(23):2765-78.
Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011 Dec 17;378(9809):2081-7. Epub 2011 Oct 27.
Centers for Disease Control and Prevention (CDC). Vital signs: Colorectal cancer screening, incidence, and mortality—United States, 2002-2010. MMWR Morb Mortal Wkly Rep. 2011 Jul 8;60(26):884-9.
Chan AT, Ogino S, Fuchs CS. Aspirin use and survival after diagnosis of colorectal cancer. JAMA. 2009 Aug 12;302(6):649-58.
Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. N Engl J Med. 2008 Mar 13;358(11):1160 74.
Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, et al. Colorectal cancer. Lancet. 2010 Mar 20;375(9719):1030-47.
Cuzick J, Otto F, Baron JA, Brown PH, Burn J, Greenwald P, et al. Aspirin and non-steroidal anti-inflammatory drugs for cancer prevention: an international consensus statement. Lancet Oncol. 2009 May;10(5):501-7.
Dahm CC, Keogh RH, Spencer EA, Greenwood DC, Key TJ, Fentiman IS, et al. Dietary fiber and colorectal cancer risk: a nested case-control study using food diaries. J Natl Cancer Inst. 2010 May 5;102(9):614-26. Epub 2010 Apr 20.
Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010 Feb 1;116(3):544-73.
Jonker DJ, O'Callaghan CJ, Karapetis CS, Zalcberg JR, Tu D, Au HJ, et al. Cetuximab for the treatment of colorectal cancer. N Engl J Med. 2007 Nov 15;357(20):2040-8.
Karapetis CS, Khambata-Ford S, Jonker DJ, O'Callaghan CJ, Tu D, Tebbutt NC, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008 Oct 23;359(17):1757-65.
Kirkegaard H, Johnsen NF, Christensen J, Frederiksen K, Overvad K, Tjønneland A. Association of adherence to lifestyle recommendations and risk of colorectal cancer: a prospective Danish cohort study. BMJ. 2010 Oct 26;341:c5504. doi: 10.1136/bmj.c5504.
Larsson SC, Orsini N, Wolk A. Vitamin B6 and risk of colorectal cancer: a meta-analysis of prospective studies. JAMA. 2010 Mar 17;303(11):1077-83.
Lieberman DA. Clinical practice. Screening for colorectal cancer. N Engl JMed. 2009 Sep 17;361(12):1179-87.
Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR; United States Multi-Society Task Force on Colorectal Cancer. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012 Sep;143(3):844-57. Epub 2012 Jul 3.
Qaseem A, Denberg TD, Hopkins RH Jr, Humphrey LL, Levine J, Sweet DE, et al. Screening for colorectal cancer: a guidance statement from the American College of Physicians. Ann Intern Med. 2012 Mar 6;156(5):378-86.
Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM; American College of Gastroenterology. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009 Mar;104(3):739-50. Epub 2009 Feb 24.
Rothwell PM, Wilson M, Price JF, Belch JF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet. 2012 Apr 28;379(9826):1591-601. Epub 2012 Mar 21.
Smith RA, Cokkinides V, Brooks D, Saslow D, Brawley OW. Cancer screening in the United States, 2010: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2010 Mar-Apr;60(2):99-119.
U.S. Preventive Services Task Force. Routine aspirin or nonsteroidal anti-inflammatory drugs for the primary prevention of colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2007 Mar 6;146(5):361-4.
U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008 Nov 4;149(9):627-37. Epub 2008 Oct 6.
|
Review Date:
12/21/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |








