Ulcerative colitis
Highlights
Ulcerative Colitis
Ulcerative colitis and Crohn's disease are inflammatory bowel diseases. All inflammatory bowel diseases cause chronic inflammation in the digestive system. Ulcerative colitis occurs only in the inner lining of the large intestine whereas Crohn's disease extends into deeper areas of the intestinal wall and can affect any part of the gastrointestinal tract (digestive system).
Causes and Risk Factors
The exact causes of ulcerative colitis are unknown.
- Genetics plays some role. Between 10 - 20% of people with ulcerative colitis have family members with the disease.
- Ulcerative colitis is diagnosed most often in people ages 15 - 35.
- Ulcerative colitis is more common among whites than people of other races. Jewish people of Eastern European (Ashkenazi) descent have a higher than average risk for developing this disease.
Symptoms
The symptoms of ulcerative colitis depend in part on how widespread the disease is and the severity of the inflammation. Common symptoms include:
- Diarrhea
- Rectal bleeding
- Difficulty or pain when passing stool
- Abdominal cramps
Prognosis
About half of patients with ulcerative have mild symptoms while another half go on to develop more severe forms of the disease. Some patients go into remission after a single attack, while others develop a chronic condition.
Treatment
There is no cure for ulcerative colitis, aside from surgical removal of the colon, but medications and dietary measures can help suppress the inflammatory response and control symptoms. Drugs used to treat ulcerative colitis include aminosalicylates (5-ASAs), corticosteroids, immunosuppressants, and biologic drugs. Some patients with ulcerative colitis are not helped by drugs and require surgical treatment.
Drug Approval
In 2012, the Food and Drug Administration (FDA) approved adalimumab (Humira) to treat moderate-to-severe ulcerative colitis that has not been helped by other drugs. Adalimumab is a biologic drug that blocks tumor necrosis factor (TNF), a protein involved in the inflammatory process. Adalimumab is also approved to treat Crohn’s disease. Like all TNF blockers, adalimumab can increase the risk for serious infections.
Introduction
Inflammatory bowel disease (IBD) is a general term that includes two main disorders:
- Ulcerative colitis
- Crohn's disease
These two diseases are related, but they are considered separate disorders with somewhat different treatment options. The basic distinctions between UC and CD are location and severity. However, some patients with early-stage IBD have features and symptoms of both disorders. (This is called indeterminate colitis.)
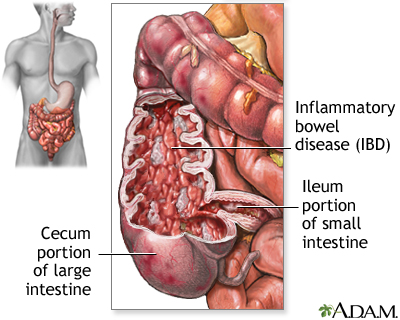
Ulcerative Colitis. Ulcerative colitis occurs only in the large intestine. Ulcers form in the inner lining, or mucosa, of the colon or rectum, often resulting in diarrhea, which may be accompanied by blood and pus. The inflammation is generally most severe in the sigmoid and rectum and usually diminishes higher in the colon. It is divided into divided into different categories depending on the location of the disease. The three main types of ulcerative colitis are:
- Proctitis. Disease only in the rectum (the lower part of the colon that connects with the anus). In about a third of patients, ulcerative colitis begins with ulcerative proctitis.
- Limited or Distal Colitis. Disease in the left side of the colon.
- Pancolitis. Disease in entire colon.
Crohn's Disease. Crohn's disease is an inflammation that extends into the deeper layers of the intestinal wall. It is found most often in the area connecting the small and large intestines, specifically in the ileum and the cecum, which is sometimes referred to as the ileocecal region. Less often, Crohn's disease occurs in other parts of the gastrointestinal tract, including the anus, stomach, esophagus, and even the mouth. It may affect the entire colon, form a string of connected ulcers in one part of the colon, or develop as multiple scattered clusters of ulcers skipping healthy tissue in between. [For more information, see In-Depth Report #103: Crohn's disease.]
The Gastrointestinal Tract
The gastrointestinal (GI) tract (the digestive system) is a tube that extends from the mouth to the anus. It is a complex organ system that first carries food from the mouth down the esophagus to the stomach and then through the small and large intestine to be excreted through the rectum and anus.
Esophagus. The esophagus, commonly called the food pipe, is a narrow muscular tube, about 9 1/2 inches long that begins below the tongue and ends at the stomach.
Stomach. In the stomach, acids and stomach motion break food down into particles small enough so that nutrients can be absorbed by the small intestine.
Small Intestine. The small intestine, despite its name, is the longest part of the gastrointestinal tract and is about 20 feet long. Food that passes from the stomach into the small intestine first passes through three parts:
- First it enters the duodenum
- Then the jejunum, and
- Finally the ileum
Most of the digestive process occurs in the small intestine.
Large Intestine. Undigested material, such as plant fiber, is passed next to the large intestine, or colon, mostly in liquid form. The colon is wider than the small intestine but only about 6 feet long. The colon absorbs excess water and salts into the blood. The remaining waste matter is converted to feces through bacterial action. The colon is a continuous structure but it is characterized as having several components
Cecum and Appendix. The cecum is the first part of the colon and it gives rise to the appendix. These structures are located in the lower-right quadrant of the abdomen. The colon continues onward in several sections:
- The first section, the ascending colon, extends upward from the cecum on the right side of the abdomen.
- The second section, the transverse colon, crosses the upper abdomen to the left side.
- The third section extends downward on the left side of the abdomen toward the pelvis and is called the descending colon.
- The final section is the sigmoid colon.
Rectum and Anus. Feces are stored in the descending and sigmoid colon until they pass through the rectum and anus. The rectum extends through the pelvis from the end of the sigmoid colon to the anus.
Causes
Doctors do not know exactly what causes inflammatory bowel disease. IBD appears to be due to an interaction of many complex factors including genetics, impaired immune system response, and environmental triggers. The result is an abnormal immune system reaction, which in turn causes an inflammatory response in the body’s intestinal regions. Ulcerative colitis and Crohn’s disease, like other IBDs, are considered autoimmune disorders.
The Inflammatory Response
An inflammatory response occurs when the body tries to protect itself from what it perceives as invasion by a foreign substance (antigen). Antigens may be viruses, bacteria, or other harmful substances.
In Crohn’s disease and ulcerative colitis, the body mistakenly targets harmless substances (food, beneficial bacteria, or the intestinal tissue itself) as harmful. To fight infection, the body releases various chemicals and white blood cells, which in turn produce byproducts that cause chronic inflammation in the intestinal lining. Over time, the inflammation damages and permanently changes the intestinal lining.
Genetic Factors
Although the exact causes of inflammatory bowel disease are not yet known, genetic factors certainly play some role. Between 10 - 20% of people with ulcerative colitis have family members with the disease. Several identified genes and chromosome locations play a role in the development of ulcerative colitis, Crohn's disease, or both. Genetic factors appear to be more important in Crohn's disease, although there is evidence that both conditions have some genetic defects in common.
Environmental Factors
Inflammatory bowel disease is much more common in industrialized nations, urban areas, and northern geographical latitudes. It is not clear how or why these factors increase the risk for IBD.
It could be that “Western” lifestyle factors (smoking, exercise, diets high in fat and sugar, stress) play some role. However, there is no strong evidence that diet or stress cause Crohn’s disease or ulcerative colitis, although they can aggravate the conditions.
Risk Factors
About 1 million Americans suffer from inflammatory bowel disease (IBD), and about half of these patients have ulcerative colitis. There are several risk factors for ulcerative colitis.
Age
Ulcerative colitis can occur at any age, but it is most often diagnosed in people ages 15 - 35 and, less commonly, in people ages 50 - 75.
Gender
Men and women are equally at risk for developing ulcerative colitis.
Family History
Ulcerative colitis tends to run in families, with up to 20% of patients having a close relative who also has the disease.
Race and Ethnicity
Ulcerative colitis is more common among whites than non-whites. Jewish people of Ashkenazi (Eastern European) descent have a heightened risk for ulcerative colitis.
Smoking
Smoking appears to decrease the risk of developing ulcerative colitis. (Because of the hazards of smoking, however, it should never be used to protect against ulcerative colitis.) Conversely, smoking appears to increases the risk of developing Crohn's disease, and can worsen the course of the disease.
Appendectomy
Removal of the appendix (appendectomy) may be linked to a reduced risk for developing ulcerative colitis, but an increased risk for Crohn’s disease.
Symptoms
The two major inflammatory bowel diseases, ulcerative colitis and Crohn's disease, share certain characteristics:
- Symptoms usually appear in young adults.
- Symptoms can develop gradually or have a sudden onset.
- Both are chronic. In either disease, symptoms may flare up (relapse) after symptom-free periods (remission) or symptoms may be continuous without treatment.
- Symptoms can be mild or very severe and disabling.
The symptoms of ulcerative colitis depend in part on how widespread the disease is and the severity of the inflammation. Common symptoms include:
- Diarrhea
- Rectal bleeding and bloody stool
- Difficulty or pain when passing stool
- Abdominal cramps
Other Symptoms
Eyes. Inflammation in the pigmented part of the eye, a condition called uveitis, is a common complication.
Joints. There is a fairly strong association with seronegative spondyloarthropathies (psoriatic arthritis, ankylosing spondylities, and other disorders). These forms of arthritis involve joints of the limbs and the spine.
Skin Disorders. Patients with ulcerative colitis have a higher risk for skin disorders and may experience an ulcerative rash called pyoderma gangrenosum that tends to heal in the center but continue to spread. Patients may also have mouth sores.
Other symptoms may include:
- Fever
- Nausea
- Loss of appetite and weight loss
- Fatigue
Prognosis. About half of patients with ulcerative colitis have mild symptoms while another half go on to develop more severe forms of the disease. Patients with more severe ulcerative colitis tend to respond less well to medications.
The course of ulcerative colitis is unpredictable. Some patients go into remission after a single attack, while others develop a chronic condition. There is no cure for ulcerative colitis (aside from surgical removal of the colon), but medications can help suppress the inflammatory response and control symptoms.
Complications
Complications in the Intestine
Malabsorption and Malnutrition. Malabsorption is the inability of the intestines to absorb nutrients. In IBD, this occurs as a result of bleeding and diarrhea, as a side effect from some of the medications, and as a result of surgery. Malnutrition may occur in ulcerative colitis, but it tends to be less severe than with Crohn’s disease.
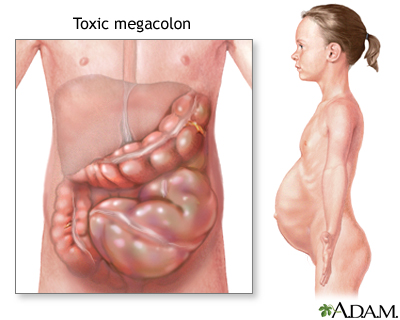
Toxic Megacolon. Toxic megacolon is a serious complication that can occur if inflammation spreads into the deeper layers of the colon. In such cases, the colon enlarges and becomes paralyzed. In severe cases, it may rupture, which is a life-threatening event requiring emergency surgery. Symptoms include weakness and abdominal pain and bloating.
Bleeding and Anemia. Rectal bleeding due to ulcers in the colon is a common complication of ulcerative colitis. It can increase the risk for anemia (reduced red blood cell count). In some cases, internal bleeding can be massive and dangerous, requiring surgery.
Intestinal Infections. Inflammatory bowel disease can increase patients’ susceptibility to Clostridium difficile, a species of intestinal bacteria that causes severe diarrhea. It is usually acquired in a hospital. However, several recent studies indicate that C. difficile is increasing among patients with inflammatory bowel disease and that many patients acquire this infection outside of the hospital setting. Patients with ulcerative colitis are at particularly high risk.
Colorectal Cancers. Inflammatory bowel disease increases the risk for colorectal cancer. The risk is highest for patients who have had the disease for at least 8 years or who have extensive areas of colon involvement. The more severe the disease, and the more it has spread throughout the colon, the higher the risk. Having a family history of colorectal cancer also increases risk.
If you have an IBD, discuss with your doctor how often you should have a colonoscopy (screening test for colorectal cancer). Current guidelines recommend that patients receive an initial colonoscopy within 8 years after IBD is diagnosed, and have follow-up colonoscopies every 1 - 2 years. The colonoscopy should include biopsies to test for dysplasia (pre-cancerous changes in cells). [For more information, see In-Depth Report #55: Colon and rectal cancers.]
Complications outside the Intestine
Bones. Ulcerative colitis, and the corticosteroid and other immune-suppressing drugs used to treat it, can cause osteopenia (low bone density) and osteoporosis (bone loss).
Liver and Gallbladder Disorders. People with ulcerative colitis have a higher than average risk for mild but not severe liver abnormalities. There is a higher risk for primary sclerosing cholangitis, which is persistent inflammation of the bile duct that can later cause serious obstruction.
Thromboembolism (Blood Clots). People with inflammatory bowel disease are at higher risk for blood clots, especially deep venous thrombosis where blood clots form in the legs. They are also at risk for pulmonary embolism, when a blood clot travels from the legs to the lungs.
Kidney Stones. People with ulcerative colitis have an increased risk for kidney stones.
Delayed Growth and Development in Children. Children with ulcerative colitis are at slightly higher than average risk for delayed growth, but their risk is lower than with Crohn's disease.
Emotional Factors. The emotional consequences of ulcerative colitis are often difficult. Eating becomes associated with fear of abdominal pain before the end of the meal. Frequent attacks of diarrhea can cause such a strong sense of humiliation that social isolation and low self-esteem may result. Ulcerative colitis takes a serious toll on work, family, and social activities. Adolescents with IBD may have added problems that increase emotional distress, including weight gain from steroid treatments and delayed puberty.
Diagnosis
There is no definitive diagnostic test for ulcerative colitis. A doctor will diagnose ulcerative colitis based on medical history and physical examination, and the results of laboratory, imaging, and endoscopic tests, which usually include biopsies of colon tissue.
Laboratory Tests
- Blood tests are used for various purposes, including to determine the presence of anemia (low red blood cell count). An increased number of white blood cells or elevated levels of inflammatory markers such as C-reactive protein may indicate the presence of inflammation.
- A stool sample may be taken and examined for blood, infectious organisms, or both.
Endoscopy
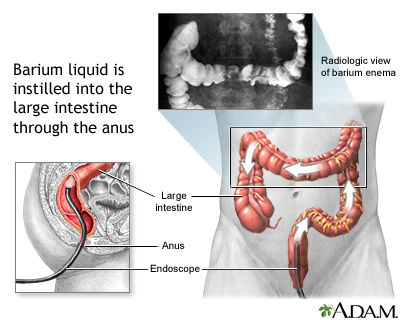
Flexible Sigmoidoscopy and Colonoscopy. Flexible sigmoidoscopy and colonoscopy are standard endoscopic procedures for diagnosing ulcerative colitis. They are important in the diagnosis of both ulcerative colitis and Crohn's disease. Both procedures involve snaking a fiber-optic tube called an endoscope through the rectum to view the lining of the colon. The doctor may also insert instruments through the endoscope to remove a tissue sample for a biopsy.
- Sigmoidoscopy, which is used to examine the rectum and left (sigmoid) colon, lasts about 10 minutes and is done without sedation. It may be mildly uncomfortable, but it is not painful. Ulcerative colitis almost always involves the lower left colon and rectum. The doctor usually observes an evenly distributed inflamed surface lining the intestine, and the bowel wall bleeds easily when touched with a swab. If sigmoidoscopy indicates ulcerative colitis, the doctor may order a colonoscopy to confirm the diagnosis and to identify how much of the colon is involved.
- Colonoscopy allows a view of the entire colon and requires a sedative, but it is still a painless procedure performed on an outpatient basis. It is helpful for distinguishing between Crohn's disease and ulcerative colitis and in screening for colon cancer.
Patients diagnosed with ulcerative colitis may also need periodic endoscopies to evaluate their condition when symptoms flare up.
Barium Enema X-Ray
Sigmoidoscopy and colonoscopy are standard tests for diagnosing ulcerative colitis, but in some cases the doctor may order a double-contrast barium enema Swallowed barium passes into the small intestine and shows up on an x-ray image, which may reveal inflammation and other abnormalities.
Ruling out Diseases Resembling Ulcerative Colitis
Crohn's Disease. Diarrhea associated with ulcerative colitis tends to be more severe than diarrhea caused by Crohn’s disease. Abdominal pain is more constant with Crohn’s disease than with ulcerative colitis. Fistulas (tracts between areas of the intestine or between the intestine and other organs) and strictures (scarring) are common with Crohn’s disease but very rare with ulcerative colitis. Endoscopy and imaging tests reveal more extensive involvement through the entire gastrointestinal tract with Crohn’s disease than with ulcerative colitis. Ulcerative colitis does not involve the small intestine as Crohn’s disease does
Irritable Bowel Syndrome. Irritable bowel syndrome (IBS), also known as spastic colon, functional bowel disease, and spastic colitis, may cause some of the same symptoms as inflammatory bowel disease. Bloating, diarrhea, constipation, and abdominal cramps are all symptoms of IBS. Irritable bowel syndrome is not caused by inflammation, however, and no fever or bleeding occurs. Behavioral therapy may be helpful in treating IBS. (Psychological therapy does not improve inflammatory bowel disease.)
Infectious Colitis. Infectious colitis appears very rapidly and painfully. Organisms can be identified in stool samples.
Intestinal Ischemia (Ischemic Colitis). Symptoms similar to irritable bowel syndrome can be caused by blockage of blood flow in the intestine. This is more likely to occur in elderly people.
Celiac Sprue. Celiac sprue, or celiac disease, is an intolerance to gluten (found in wheat) that triggers inflammation in the small intestine and causes diarrhea, vitamin deficiencies, and stool abnormalities. It occurs in some people with inflammatory bowel disease (IBD) and is usually first noticed in children.
Acute Appendicitis. Crohn's disease may cause tenderness in the right lower part of the abdomen, where the appendix is located, that resembles appendicitis.
Cancer. Colon or rectal cancers must always be ruled out when symptoms of IBD occur.
Treatment
Treatment can help suppress the inflammatory response and manage symptoms. A treatment plan for ulcerative colitis includes:
- Diet and nutrition
- Medications
- Surgery (when necessary)
Diet and Nutrition
Malnutrition may occur in ulcerative colitis, although it tends to be less severe than with Crohn’s disease. Patients with ulcerative colitis may experience reduced appetite and weight loss.
Patients should strive to eat a well-balanced healthy diet and focus on getting enough calories, protein, and essential nutrients from a variety of food groups. These include protein sources such as meat, chicken, fish or soy; dairy products such as milk, yogurt, and cheese (if the patient is not lactose-intolerant); and fruits and vegetables.
Depending on your nutritional status, your doctor may recommend that you take a multivitamin or iron supplement. Other types of dietary supplements, such as probiotics (“healthy bacteria” like lactobacilli), are being investigated for ulcerative colitis. Studies suggest that probiotics do not help much for remission, but they may have modest effects for reducing disease activity and improving symptoms in people with mild-to-moderate ulcerative colitis.
Certain types of foods may worsen diarrhea and gas symptoms, especially during times of active disease. While people vary in their individual sensitivity to foods, general guidelines for dietary management during active disease include:
- Eat small amounts of food throughout the day.
- Stay hydrated by drinking lots of water (frequent consumption of small amounts throughout the day).
- Eat soft, bland foods and avoid spicy foods.
- Avoid high-fiber foods (bran, beans, nuts, seeds, and popcorn).
- Avoid fatty greasy or fried foods and sauces (butter, margarine, and heavy cream).
- Limit milk products if you are lactose intolerant (or consider taking a lactase supplement to improve tolerance). Otherwise, dairy products are a good source of protein and calcium.
- Avoid or limit alcohol and caffeine consumption.
Medications
Drug therapies for ulcerative colitis aim to resolve symptoms (induce remission) and prevent flare-ups (maintain remission). The main types of drugs used for treating ulcerative colitis include:
- Aminosalicylates. Mild-to-moderate ulcerative colitis is usually treated with aspirin-like medications called aminosalicylates, or 5-ASAs. These drugs are also used to treat relapses. They may be administered rectally in patients who have mild-to-moderate disease that occurs only in the last portion of the intestine. They may also be taken by mouth.
- Corticosteroids. Corticosteroids (steroids) may be added or used alone to reduce acute inflammation. (Because of their significant side effects, they are not recommended for long-term use and maintenance therapy). Steroids may be administered rectally as an alternative to an aminosalicylate if the disease is limited to the last portion of the intestine. Forms taken by mouth may treat moderate-to-severe cases. People who do not respond to less aggressive treatments may need intravenous steroids.
- Immunosuppressants. Drugs that suppress the immune system (immunosuppressants) are useful, either alone or in combinations, for disease that does not respond to other treatments or for maintenance of remissions.
- Biologic Drugs. Biologic drugs are designed to stimulate the immune system and interfere with specific proteins (cytokines) involved with the inflammatory response. Infliximab (Remicade) is the only biologic drug approved for ulcerative colitis. It blocks a cytokine called tumor necrosis factor (TNF).
Drug therapy is considered successful if it can push the disease into remission (and keep it there) without causing significant side effects. The patient's condition is generally considered in remission when the intestinal lining has healed and symptoms such as diarrhea, abdominal cramps, and tenesmus (straining painfully to defecate) are normal or close to normal.
Other types of drugs may also be used to treat specific conditions and symptoms associated with ulcerative colitis. Anti-diarrheal medications such as loperamide (Imodium, generic) may be given to help control diarrhea.
Surgery
Drugs do not help about 25 - 40% of patients with ulcerative colitis. As a result, these people need surgical treatment. Surgery may also be necessary because of hemorrhage, perforation of the colon, or toxic megacolon.
Total proctocolectomy with ileal pouch anal anastomosis (IPAA), also known as restorative proctolectomy, and total proctocolectomy with ileostomy are the two definitive surgical approaches for widespread ulcerative colitis that cannot be controlled with medications. Other patients may have a colectomy (resection of a portion of the colon) for more limited disease.
Unlike Crohn’s disease, which can recur after bowel resection, ulcerative colitis does not recur after total proctocolectomy. Total proctocolectomy is considered a cure for ulcerative colitis. (See Surgery section for more detailed information.)
Medications
Aminosalicylates
Aminosalicylates contain the compound 5-aminosalicylic acid, or 5-ASA, which helps reduce inflammation. These drugs are used to prevent relapses and maintain remission in mild-to-moderate ulcerative colitis.
The standard aminosalicylate drug is sulfasalazine (Azulfidine, generic). This drug combines the 5-ASA drug mesalamine with sulfapyridine, a sulfa antibiotic. While sulfasalazine is inexpensive and effective, the sulfa component of the drug can cause unpleasant side effects, including headache, nausea, and rash.
Patients who cannot tolerate sulfasalazine or who are allergic to sulfa drugs have other options for aminosalicylate drugs, including mesalamine (Asacol, Pentasa, Lialda, generic),(Dipentum), and balsalazide (Colazal, generic). These drugs, like sulfasalazine, are taken as pills several times a day. Lialda is a once-daily mesalamine pill for patients with ulcerative colitis. Mesalamine is also available in enema (Rowasa, generic) and suppository (Canasa, generic) forms.
Mesalamine can cause kidney problems and should be used with caution by patients with kidney disease. Common side effects of aminosalicylate drugs include:
- Abdominal pain and cramps (mesalamine, balsalazide)
- Diarrhea (mesalamine, olsalazine)
- Gas (mesalamine)
- Nausea (mesalamine)
- Hair loss (mesalamine)
- Headache (mesalamine, balsalazide)
- Dizziness (mesalamine)
All mesalamine preparations, including sulfasalazine, appear to be safe for children and women who are pregnant or nursing.
Corticosteroids
Corticosteroids (commonly called steroids) are powerful anti-inflammatory drugs. They are used only for active ulcerative colitis. Steroids are frequently combined with other drugs to produce more rapid symptom relief and to allow quicker withdrawal, although such combinations do not improve remission time. Because the oral form has serious long-term effects, they are not useful for maintenance therapy. Patients who have a poor response to steroids are also less likely to do well with repeat therapy.
Corticosteroid Types. Prednisone (Deltasone, generic), methylprednisolone (Medrol, generic), and hydrocortisone (Cortef, generic) are the most common oral corticosteroids. Newer steroids, such as budesonide (Entocort), are given via enema and affect only local areas in the intestine and do not circulate throughout the body. Such drugs may avoid the widespread side effects that are a serious problem with long-term treatment using older conventional steroids. They are only helpful for milder ulcerative colitis involving the rectum and sigmoid colon.
Administering Corticosteroids. Most corticosteroids can be taken as a pill. For patients who cannot take oral forms, methylprednisolone and hydrocortisone may also be given intravenously or rectally as a suppository, enema, or foam. The severity or location of the condition often determines the form.
Side Effects of Corticosteroids. Oral steroids can have distressing and sometimes serious long-term side effects, including:
- Susceptibility to infection
- Weight gain (particularly increased fatty tissue on the face and upper trunk and back)
- Acne
- Excess hair growth
- High blood pressure (hypertension)
- Weakened bones (osteoporosis)
- Cataracts and glaucoma
- Diabetes
- Muscle wasting
- Menstrual irregularities
- Upper gastrointestinal ulcers
- Personality change, including irritability, insomnia, psychosis, and depression; such emotional changes are sometimes severe enough to produce suicidal thoughts
Withdrawing from Corticosteroids. Once the intestinal inflammation has subsided, steroids must be withdrawn very gradually. Withdrawal symptoms, including fever, malaise, and joint pain, may occur if the dosage is lowered too rapidly. If this happens, the dosage is increased slightly and maintained until symptoms are gone. More gradual withdrawal is then resumed.
Immunosuppressive Drugs
Immunosuppressant drugs are used for long-term therapy, especially for very active inflammatory bowel disease that does not respond to milder treatments. Such drugs suppress or restrain actions of the immune system and therefore the inflammatory response that causes ulcerative colitis. Immunosuppressants can prevent relapse, even when used alone, and in some studies have proved to help maintain remissions in ulcerative colitis for up to 2 years.
Azathioprine (Imuran, Azasan, generic) and mercaptopurine ([6-MP], Purinethol, generic) are the standard oral immunosuppressant drugs. However, it can take 3 - 6 months for these drugs to have an effect. To speed up the response, they are sometimes prescribed along with a corticosteroid drug. Lower steroid doses are then needed, resulting in fewer side effects. Corticosteroids may also be withdrawn more quickly. For this reason, immunosuppressants are sometimes referred to as steroid-sparing drugs.
Other pill forms of immunosuppressants include cyclosporine A (Sandimmune, Neoral) and tracrolimus (Prograf). Cyclosporine A is also given intravenously to patients with severe ulcerative colitis. These drugs are quicker-acting than azathiopine and 6-mercaptopurine. Cyclosporine A generally takes 1 - 2 weeks to take effect. Methotrexate (MTX, Rheumatrex) is another fast-acting type of injectable immunosuppressant that is effective for Crohn’s disease but not for ulcerative colitis. Antibiotics, which are used to treat Crohn's disease, are also not helpful for ulcerative colitis.
General side effects of immunosuppressants may include nausea, vomiting, and liver or pancreatic inflammation. Patients should receive frequent blood tests to monitor bone marrow, liver, and kidneys. Patients who take cyclosporine A or tacrolimus need to have their blood pressure and kidney function checked regularly. Children and young adults who take azathioprine or mercaptopurine should be monitored for signs of cancer as these drugs have been associated with increased risk of an aggressive form of T-cell lymphoma. Immunosuppressants are usually not recommended for women who are pregnant or breast-feeding.
Biologic Drugs (Infliximab)
Biologic response modifiers are genetically engineered drugs that target specific proteins involved with the body’s inflammatory response. Two biologic drugs are approved for treatment of moderate-to-severe ulcerative colitis in patients who have not responded to other drugs:
- Infliximab (Remicade), which is given by intravenous infusion in a doctor’s office or hospital clinic (after the first three doses, the drug is administered every 8 weeks)
- Adalimumab (Humira), which you can give by injection at home (after the first two doses, you give yourself an injection every other week)
Infliximab and adalimumab target and block an inflammatory immune factor known as tumor necrosis factor (TNF). These drugs are described as anti-TNF drugs, TNF blockers, or TNF inhibitors. Studies indicate that anti-TNF drugs may reduce ulcerative colitis symptoms and help patients achieve and maintain remission. .
Common side effects of TNF inhibitors include respiratory infections (sinus infections and sore throat), headache, rash, cough, and stomach pain. All anti-TNF drugs can potentially cause serious severe side effects, including increased susceptibility to viral, fungal, and bacterial infections (including tuberculosis).
Your doctor should carefully monitor you for any signs of infection. Symptoms of fungal infections include fever, malaise, weight loss, sweating, cough, and shortness of breath. If you experience any of these symptoms, contact your doctor.
Anti-TNF drugs can increase the risk for cancer, particularly lymphomas, in children and adolescents. They can also increase the risk for leukemia in patients of all ages. Other severe side effects may include psoriasis, heart failure, liver failure, aplastic anemia, nervous system disorders, and allergic reactions.
Surgery
Proctocolectomy and Ileoanal Anastomosis
Proctocolectomy is removal of the entire colon, including the lower part of the rectum and the sphincter muscles that control bowel movements. It can achieve a complete cure, but it is a last resort.
Ileostomy. In some proctocolectomies, the surgeon creates an opening in the abdominal wall (called a stoma) to allow passage of waste material. This part of the procedure is referred to as an ileostomy, and the stoma is created in the lower right corner of the abdomen. The surgeon then connects cut ends of the small intestine to this opening. An ostomy bag is placed over the opening and accumulates waste matter. It requires emptying several times a day.
Ileoanal Anastomosis. Ileal pouch anal anastomosis (IPAA), also simply called ileoanal anastomosis, has now largely replaced ileostomy because it preserves part of the anus and allows for more normal bowel movements. The procedure creates a natural pouch to collect waste, rather than using an ileostomy bag. The standard procedure involves:
- The colon is removed as in proctocolectomy, but the surgeon only strips the superficial diseased inner layer of the rectum, leaving the sphincter muscles intact.
- The anus is then attached to the ileum (the final portion of the small intestine leading to the colon).
- A pouch is constructed out of the small bowel above the anus. The pouch is able to collect waste material, and the patient can pass bowel movements normally through the anus, although they are watery and more frequent than normal (five or six times a day).
- A temporary abdominal opening (ileostomy) is usually required, but it is typically closed up in a second operation a few months later.
Managing Daily Life after Surgery
Flatulence is the most socially distressing problem following surgery. Unfortunately many of the fiber rich vegetables and whole grains that can benefit patients with ulcerative colitis can also cause gas. (Surgical patients should avoid or chew thoroughly insoluble fiber foods, such as popcorn, olives, and vegetable skins, which can obstruct the stoma.) Some pouching systems have filters that can help limit flatulence. Typically, flatulence occurs 2 - 4 hours after eating, which may help patients time their meals to ensure privacy afterward.
Patients must increase fluid intake, and include not only water but also broth, sports drinks, and vegetable juice to maintain appropriate levels of sodium and potassium.
Patients should avoid time-released, coated, or large pills, which often are not completely absorbed and may block the stoma.
Ileostomy and ileoanal anastomosis do not interfere with bathing or showering or most physical activity. (Patients should avoid contact sports.) As a rule, the surgeries do not impair sexual function.
Outcome and Complications from Ileoanal Anastomosis
Complications are common with any intestinal operation. In about 5 - 10% of IPAA procedures, complications occur that require conversion to an ileostomy. In general, patient satisfaction is very high with this procedure. Most patients report better or much better quality of life 5 years after the procedure. Most patients can postpone their bowel movements until they are convenient. Bowel movements still average about six a day.
Pouchitis. Inflammation of the pouch (pouchitis) is the most common complication of the pouch procedures. Symptoms include rectal bleeding, cramps, and fever. It can usually be successfully treated with antibiotics such as metronidazole (Flagyl, generic) or ciprofloxacin (Cipro, generic).
Bowel obstruction may occur although it is less common than pouchitis. With most patients, this condition can be treated by avoiding food for several days and administering intravenous fluids. In about a third of patients with bowel obstruction, surgery may need to be performed to remove the blockage.
Pouch failure occurs in a small percentage of patients. It requires permanent removal of the pouch and use of ileostomy.
Irritable Pouch Syndrome. Irritable pouch syndrome is a problem that includes frequent bowel movements, an urgent need to defecate, and abdominal pain. There are no signs of inflammation, however, as there are with pouchitis. Stress and diet play a role in this condition, and it is usually relieved after a bowel movement.
Infertility. IPAA triples the risk of infertility in women with ulcerative colitis. The surgery may cause scarring or blocking of fallopian tubes, which increases the risk of infertility. About half of women who undergo this procedure become infertile.
Resources
- www.ccfa.org -- Crohn's & Colitis Foundation of America
- www.gastro.org -- American Gastroenterological Association
- www.acg.gi.org -- American College of Gastroenterology
- www2.niddk.nih.gov -- National Digestive Diseases Information Clearinghouse
References
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009 Nov 19;361(21):2066-78.
Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, et al. World Gastroenterology Organization Practice Guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010 Jan;16(1):112-24.
Burger D, Travis S. Conventional medical management of inflammatory bowel disease. Gastroenterology. 2011 May;140(6):1827-1837.e2..
Clark M, Colombel JF, Feagan BC, Fedorak RN, Hanauer SB, Kamm MA, et al. American gastroenterological association consensus development conference on the use of biologics in the treatment of inflammatory bowel disease, June 21-23, 2006. Gastroenterology. 2007 Jul;133(1):312-39.
Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011 Nov 3;365(18):1713-25.
Farraye FA, Odze RD, Eaden J, Itzkowitz SH, McCabe RP, Dassopoulos T, et al. AGA medical position statement on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010 Feb;138(2):738-45.
Ford AC, Achkar JP, Khan KJ, Kane SV, Talley NJ, Marshall JK, et al. Efficacy of 5-aminosalicylates in ulcerative colitis: systematic review and meta-analysis. Am J Gastroenterol. 2011 Apr;106(4):601-16. Epub 2011 Mar 15.
Ford AC, Bernstein CN, Khan KJ, Abreu MT, Marshall JK, Talley NJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011 Apr;106(4):590-9; quiz 600. Epub 2011 Mar 15.
Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011 Apr;106(4):644-59, quiz 660. Epub 2011 Mar 15.
Holubar SD, Cima RR, Sandborn WJ, Pardi DS. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst Rev. 2010 Jun 16;6:CD001176.
Khan KJ, Dubinsky MC, Ford AC, Ullman TA, Talley NJ, Moayyedi P. Efficacy of immunosuppressive therapy for inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. 2011 Apr;106(4):630-42. Epub 2011 Mar 15.
Kornbluth A, Sachar DB; Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010 Mar;105(3):501-23; quiz 524. Epub 2010 Jan 12.
Mahid SS, Minor KS, Soto RE, Hornung CA and Galandiuk S. Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clin Proc. 2006;81(11):1462-71.
Mallon P, McKay D, Kirk S and Gardiner K. Probiotics for induction of remission in ulcerative colitis. Cochrane Database Syst Rev. 2007;(4):CD005573.
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012 Jan;142(1):46-54.e42. Epub 2011 Oct 14.
Mowat C, Cole A, Windsor A, Ahmad T, Arnott I, Driscoll R, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011 May;60(5):571-607.
Rutgeerts P, Vermeire S, Van Assche G. Biological therapies for inflammatory bowel diseases. Gastroenterology. 2009 Apr;136(4):1182-97. Epub 2009 Feb 26.
Thomas DW, Greer FR; American Academy of Pediatrics Committee on Nutrition; American Academy of Pediatrics Section on Gastroenterology, Hepatology, and Nutrition. Probiotics and prebiotics in pediatrics. Pediatrics. 2010 Dec;126(6):1217-31. Epub 2010 Nov 29.
Timmer A, Preiss JC, Motschall E, Rücker G, Jantschek G, Moser G. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2011 Feb 16;(2):CD006913.
|
Review Date:
12/21/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |












