Vasectomy and vasectomy reversal
Highlights
Vasectomy
Vasectomy is a safe and effective surgical operation for male sterilization, a permanent form of birth control. Vasectomy works by interrupting the route that the sperm take from the testicles (where they are produced) to the penis. After vasectomy, the testicles still continue to generate sperm, but their movement is blocked at the site of the vasectomy. Vasectomy does not affect a man's ability to perform sexually, or his sexual satisfaction. It does not change male hormones, male sex characteristics, the sex drive, or semen production.
Vasectomy Surgery
Vasectomy surgery is a much simpler operation than female sterilization. It usually takes 15 - 30 minutes to perform and is done at a doctor’s office or family planning clinic. Local anesthesia is used and the patient can return home the same day.
After Surgery
Patients will feel sore for a few days, but discomfort can be reduced by pain relievers (analgesics) and an ice pack. Normal activities can be resumed within a few weeks. For the first few months after the vasectomy, some active sperm are delivered to the semen so additional contraceptive measures are needed until a semen analysis confirms absence of live sperm.
It takes, on average, about 3 months to clear the viable sperm from the reproductive system. The doctor will perform a semen analysis at about 12 weeks after vasectomy to verify that no live sperm remain in the semen. It is essential that the patient and his partner continue to use other methods of birth control until his sperm count is zero.
Vasectomy Reversal
The decision to have a vasectomy should be carefully considered. A reversal procedure can be performed, but it does not guarantee restored fertility. In addition, these reversal procedures (vasovasostomy and vasoepididymostomy) are much more complicated surgeries than vasectomy.
American Urological Assocation Guidelines
In 2012, the American Urological Assocation (AUA) released guidelines for vasectomy. The AUA recommends that a man considering a vasectomy should meet with the doctor for a pre-operative consultation. The AUA emphasizes that it’s important for men to understand that vasectomy is intended as a permanent form of contraception.
Introduction
In the United States, vasectomy emerged as a popular method of permanent contraception during the 1960s. Within a decade, 750,000 men were undergoing vasectomies each year. Vasectomy rates markedly declined in the 1990s and have now leveled off at about 500,000 a year. Worldwide, millions of couples use vasectomy as a method of permanent birth control. [For non-permanent methods of birth control, including condoms, see In-Depth Report #91: Birth control options for women. ]
The procedure works by surgically interrupting the route that the sperm take from the testicles (where they are produced) to the penis. After vasectomy, the testicles still continue to generate sperm, but their movement is blocked at the site of the vasectomy. Eventually the sperm die, and the body naturally absorbs them. During sex, semen is produced in the same amount as before vasectomy, but this fluid does not contain sperm.
Vasectomy should not be confused with castration. It does not affect a man's ability to perform sexually, or on his sensation of orgasm and pleasure. It does not change male hormones, male sex characteristics, or sex drive. Testosterone continues to be produced in the testes and delivered into the bloodstream. Sperm form a very small portion of semen, so patients notice no difference in the amount of semen produced during orgasm.
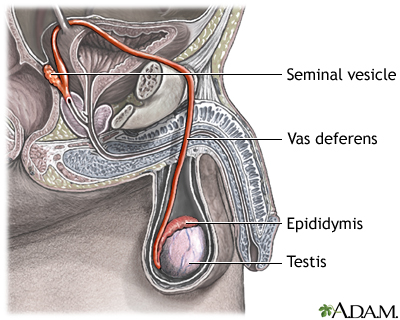
The Male Reproductive Tract
The male reproductive tract performs three functions:
- It enables a man to produce offspring.
- It provides him with a supply of male hormones.
- It enables him to experience sexual pleasure.
The Traveling Sperm. The sperm's journey through the male body -- from the testes (the testicles) to the final stage (the orgasm) -- is long and complex:
- Sperm are produced in the testes at a rate of 50,000 an hour within tiny ducts called seminiferous tubules.
- Sperm do not mature in the testes. They must first pass into the epididymis, a C-shaped storage chamber adjoining the testes composed of a 20-foot coiled tube. The sperms' journey through the epididymis takes about 2 - 3 weeks. They are held here until sexual activity forces them to move on.
- When a man experiences sexual excitement, nerves stimulate the muscles in the epididymis to contract. This forces the sperm to pass into one of two rigid and wire-like muscular channels, called the vasa deferentia. (A single channel is called a vas deferens. It is the vas deferens that is cut during vasectomy.)
- Muscle contractions in the vas deferens from sexual activity propel the sperm along past the seminal vesicles, which are clusters of tissue that contribute fluid, called seminal fluid, to the sperm. The vas deferens also collects fluid from the nearby prostate gland. This mixture of various fluids and sperm is the semen.
- Each vas deferens then joins together to form the ejaculatory duct. This duct, which now contains the sperm-containing semen, passes down through the urethra. (The urethra is the same channel in the penis through which a man urinates. During orgasm, however, the bladder neck closes so urine cannot enter the urethra.)
- The semen is forced through the urethra during ejaculation, the final stage of orgasm when the sperm are literally ejected from the penis.
The decision to have a vasectomy should be made only after serious consideration. The surgery is intended to be permanent. Most men who seek a vasectomy have been married for 10 years or more. Not all are good candidates, however. It is important that both the woman and the man completely agree that they no longer want to have children. They should also agree that permanent birth control is the right decision for them. Ideally, the couple should view the operation as a mutual commitment to an already successful marriage or relationship. Vasectomy is generally not a good idea if the couple's relationship is under great stress. It is not a cure for emotional or sexual problems between a man and woman.
Single men, some of them younger, may also choose to have a vasectomy. Doctors may refuse to perform the procedure depending on how young the person is, or they may ask these men to wait for a year or even more.
Treatment
After deciding that permanent birth control is the best solution, a couple still has the option of either vasectomy for the male or tubal ligation (female sterilization) for the female. Female sterilization is performed three times as often as vasectomy, but vasectomy is a less complicated and less expensive procedure, and poses fewer risks for complications. [For more information, see In-Depth Report #91: Birth control options for women.]
Vasectomy is very safe and is nearly 100% effective for preventing pregnancy. It does not protect against sexually transmitted diseases (STDs). Condoms remain the best method of STD prevention for sexually active people.
The decision to have a vasectomy should be carefully considered. A reversal procedure can be performed, but it is a major operation that does not guarantee restored fertility. In addition, these reversal procedures (vasovasostomy and vasoepididymostomy) are much more complicated surgeries than vasectomy.
After-Effects
Surveys indicate that most men are satisfied with vasectomy and that this satisfaction persists. Men who have vasectomies usually feel relieved that the worry about pregnancy is over, and most couples respond well to their new-found contraceptive freedom.
Vasectomy does not affect a man's hormonal levels and does not impair sexual potency, desire, or satisfaction. Some men may go through a brief period of self-consciousness, wondering whether others notice some difference in their masculinity. For most men, this tentativeness passes quickly. Some couples may experience difficulties, which manifest in sexual dysfunction such as erectile dysfunction, premature ejaculation, or painful intercourse. In such cases, the underlying cause is usually unresolved emotional issues, not the vasectomy itself.
Who Should Have a Vasectomy
Vasectomies may be right for:
- Men in relationships in which both partners agree they have all the children they want and both do not want to use or are unable to use other methods of contraception
- Men in relationships whose partners have health problems that make pregnancy unsafe
- Men in relationships in which one or both have genetic disorders that they do not want to transmit to their offspring
Vasectomies may not be right for:
- Men in relationships in which one partner is unsure about his or her desire to have children in the future
- Men whose current relationships are unstable, going through a stressful phase, or are marked by substantial conflict
- Men who are considering the operation just to please their partners
- Men who are counting on having children later by storing sperm or by surgical reversal of the vasectomy
- Young men, who still have many life changes ahead
- Men who are single (including those divorced or separated) at the time of vasectomy
- Men or couples whose only motive is freedom from distraction imposed by other contraceptive methods during sexual activity
Sperm Banking
Sperm banking can be used in conjunction with vasectomy or vasectomy reversal surgery. Sperm banking involves freezing (cryopreservation) and storage (cryobanking) of sperm. It is usually performed before a vasectomy, or during or after reversal surgery. If a man later desires to have children, the sperm can be used for assisted reproductive technologies, usually intracytoplasmic sperm injection (ICSI) used in combination with in vitro fertilization. [For more information, see In-Depth Report #67: Infertility in men.]
Sperm banking is no guarantee for successful conception and pregnancy. Sperm can be frozen for many years, but even after 6 months some sperm cells lose their ability to function normally after being unfrozen. In addition, sperm banking is typically not covered by health insurance plans and costs should be considered.
Although most men who have a vasectomy never use their banked sperm, it is understandable if some men are emotionally reassured by the idea that they have sperm preserved "just in case." Still, men who are considering vasectomy should not view sperm banking (or vasectomy reversal) as a guaranteed option if they later change their minds. It is best to undertake vasectomy as a permanent sterilization procedure. If future fathering of children seems a possibly desirable scenario, it is wise to reconsider whether vasectomy is the right decision to make.
Vasectomy Surgery
Vasectomy is a minor operation that takes about 15 - 30 minutes and is usually performed with local anesthesia in a doctor's office or a family planning clinic. Most insurance policies will cover vasectomies performed as a minor outpatient procedure, but will not cover vasectomies performed as major surgery in an operating room. If a Vasclip procedure is performed, there may be an additional cost for this device.
Conventional Vasectomy
A conventional vasectomy procedure is performed as follows:
- To prevent increased risk of bleeding, patients should avoid taking aspirin or NSAIDs [including ibuprofen (Advil, generic) and naproxen (Aleve, generic)] for several days prior to the procedure.
- Before the operation, the patient's scrotum is shaved and cleaned.
- A local anesthetic is injected into the skin of the scrotum over where the vasectomy will take place. An anesthetic cream may be applied before the injection to reduce its pain.
- The surgeon makes a tiny incision on one side of the scrotum and locates one vas deferens. The vas deferens is isolated, drawn through the incision, and clamped at two sites close to each other.
- The segment between the clamps (which should be more than 15 mm, or a little over 1/2 inch) is then removed.
- The surgeon then seals off (ligates) the tube with sutures and cauterizes it with an electric needle. Fascial interposition is an additional technique that may be used in combination with these methods to improve chance of permanent closure. With fascial interposition, the surgeon pulls the fibrous layer covering the vas (the fascia) over the cut end of the vas and sews it closed. This increases the barrier and further reduces residual sperm. Research suggests that cauterization, with or without fascial interposition, is the best method for sealing off the vas.
- The surgeon may choose to close off either one end of the vas (called an open-ended procedure) or both ends (closed-ended technique). In the open-ended procedure, the vas section connected to the testis is left open, and the one leading to the prostate is sealed. In the closed-ended approach, both are sealed. Many surgeons prefer the open-ended version because it has lower complication and failure rates than the closed-ended method, and it results in fewer cases of chronic pain.
- After closing off the tube, the vas deferens is gently placed back into the scrotum.
- The procedure is then repeated on the other side.
- After a short rest, usually about half an hour, the patient can leave the doctor's office or clinic. Arrangements should be made ahead of time for someone to drive the patient home.
No-Scalpel Vasectomy
Minimally-invasive techniques are now the preferred methods for vasectomy. The first of these, called no-scalpel vasectomy (NSV), has been in use since 1974. As its name implies, NSV does not require a scalpel or incisions.
The technique takes about 10 minutes and is performed in a doctor's office or a family planning clinic. The no-scalpel vasectomy differs from a conventional vasectomy in the method of accessing the vasa deferentia:
- In NSV, the doctor feels for the vas deferens under the skin and holds them in place with a small ring clamp.
- Instead of making two incisions, the doctor uses a sharp hemostat, a special instrument that makes one tiny puncture and then is used to gently stretch the opening until the vas deferens can be pulled through it. (The surgeon must rotate his wrist to pull the vas out -- called a supination maneuver -- which may be difficult to perform.)
- The vas is then sealed off using the same methods (clips, sutures, cauterization using an electric needle, or some combination) as conventional vasectomy. As with standard vasectomy, the closures can be open- or closed-ended.
- There is very little bleeding with the no-scalpel vasectomy. No stitches are needed to close the tiny opening, which heals quickly and leaves no scar.
When performed correctly, NSV works just as well as conventional vasectomy, takes less time, and causes less bleeding, infection, and pain. Current research indicates that NSV is the safest type of vasectomy procedure. NSV is difficult to perform, however, and most surgeons must do about 15 - 20 procedures in order to be proficient. NSV is becoming a popular alternative to standard vasectomy, but it is important to select a doctor who is experienced with this procedure.
A simpler method of NSV, called percutaneous vasectomy, is now also being used. Recent research suggests that it works as well as standard NSV and is easier to perform. Percutaneous vasectomy uses the same instruments as no-scalpel vasectomy, but with a different surgical technique. The hemostat is used to first puncture the skin (instead of spearing the vas and lifting it out). The ringed clamp is then passed through the incision and used to enclose the section of the vas that is then pulled out for closure. This avoids the need for the difficult wrist maneuver in NSV.
Other Vasectomy Procedures
Vasclip. The Vasclip is a newer alternative to conventional vasectomy. The procedure does not involve cutting the vas deferens. Instead, a very small rice-sized plastic clip is locked around the vas deferens to stop the flow of sperm. Some studies have reported fewer post-surgical complications than with standard vasectomy, including infection and swelling. However, studies have also reported that the Vasclip is less effective than no-scalpel vasectomy for reducing sperm count. To date, there is insufficient evidence that the Vasclip is better than standard vasectomy. Some insurance companies consider this procedure to be investigational and will not pay for it.
Recovery
Vasectomy is a low-risk procedure, and complications, which occur in about 10% of patients, are usually easy to control. There are generally fewer complications with no-scalpel vasectomy. Pain or soreness typically lingers for a few days after the procedure, but this is normal and usually does not require a return visit to the doctor. No deaths resulting from vasectomy have ever been reported in the United States.
Nearly all men recover completely in a few days. The following are some guidelines after the operation to help recovery:
- The local anesthetic wears off about 1 - 2 hours after the procedure, and most patients then experience a dull ache in the testicles and groin. The doctor may prescribe a painkiller for the first few days, continuing with mild over-the-counter pain relievers if discomfort persists. Acetaminophen (Tylenol, generic) with or without codeine is the primary choice for postoperative pain. Aspirin, ibuprofen (Advil, Motrin, generic), naproxen (Aleve, generic), or other non-steroidal anti-inflammatory drugs (NSAIDs) can cause bleeding and should be avoided.
- The patient should stay in bed on his back for at least one day and apply ice packs for 8 hours. The doctor may suggest that the patient wear an athletic supporter.
- Some oozing of blood onto the gauze pads is normal during the first 2 days after the operation.
- The patient should not perform any heavy physical labor for at least 2 days. Sports and heavy lifting may be resumed 2 - 3 weeks after surgery.
- Men can resume having sex about a week after surgery, but should use contraception until a semen analysis confirms that no functional sperm remain. During ejaculation, the patient may experience some discomfort in the groin and testicles at first due to the contraction of the vas deferens. This sensation diminishes as the tissues heal.
Although rare, more serious complications may occur soon after surgery. They include:
Bleeding. Blood may seep under the skin, so that the scrotum and penis appear to be bruised. If there is no dangerous swelling, this painless and common problem usually disappears without treatment within 1 - 2 weeks. If the bleeding is excessive and requires more than two or three gauze changes per day, call your doctor.
Hematoma. In less than 1% of cases, bleeding inside the scrotum can cause a painful swelling known as a hematoma. In these cases, the scrotum swells up shortly after vasectomy. The doctor should be called immediately.
Infection. Infection can occur after vasectomy. The incision site may become infected, causing redness and swelling around the incision. Antibiotics, antimicrobial creams or ointments, or both, along with hot baths several times a day, will usually clear the infection in a few days. Severe infections are extremely rare.
Semen Analysis
Vasectomy does not produce immediate sterility. After the vasectomy procedure, there are always some active sperm left in the semen for several months, so the risk for pregnancy persists. The patient is considered sterile only when there are no live or moving (motile) sperm in his semen.
It takes, on average, around 3 months to clear the viable sperm from the reproductive system, but it may take some men as long as 6 months to become sterile. The doctor will perform a semen analysis 8 - 16 weeks after vasectomy to verify that no live sperm remain in the semen. It is essential that the patient and his partner continue to use other methods of birth control until his sperm count is zero.
Many men who have vasectomies never bother to return for follow-up sperm testing (semen analysis). Without a follow-up test, men do not know whether the vasectomy was successful. Until test results verify that there are no sperm in the semen, men are at risk of fathering unwanted pregnancies. In addition to a lab test at the doctor’s office, there is an FDA-approved home test kit for post-vasectomy confirmation testing (SpermCheck Vasectomy).
If motile sperm are found in a sperm analysis 6 months after vasectomy, the procedure is considered a failure. Repeat vasectomy may be an option. Failed vasectomies are rare, and repeat vasectomies are needed less than 1% of the time.
Long-Term Complications
Vasectomy Failure and Unexpected Pregnancy. Pregnancy rates after a vasectomy are very low, about 1 in 1,000. There are two main reasons for an unexpected pregnancy:
- Residual sperm were still alive when the partners had unprotected sex. This is the most common reason for an unexpected pregnancy after a vasectomy. Men should make sure they have follow-up sperm analysis testing. They should also continue to use birth control until their doctor notifies them that the test results confirm sterility.
- Failure of the procedure and recanalization. Failure in some cases is due to a technical error, but most often it is due to recanalization -- when the cut ends of the vas spontaneously reconnect. Success rates are best when an experienced surgeon performs the vasectomy.
Recanalization and Sperm Granulomas. The primary reason for vasectomy failure is recanalization -- when the cut ends of the vas deferens spontaneously reconnect. Recanalization in some cases may be due to sperm granulomas. These are tiny balls of debris that form from sperm, scar tissue, and white blood cells at the incision site. Cells lining the inside of the vas deferens grow through the scar tissue and form a new channel through which the sperm can now move. In general, surgeons can reduce the risk for recanalization by leaving a gap between the two cut ends.
This natural vasectomy reversal can occur after any vasectomy surgical procedure, but it is uncommon. When recanalization does occur, sperm counts are almost always very low and pregnancies are still rare. Most cases of recanalization develop within several months after the operation. In very rare cases, sperm have reappeared a year or even longer after vasectomy.
Epididymitis. Epididymitis occurs when an inflammation at the site of the vasectomy causes swelling of the epididymis. This rare condition usually occurs within the first year and is treated with heat and anti-inflammatory medications. It usually clears up within a week.
Anti-sperm Antibodies. Sperm continue to be produced after vasectomy but are disposed of in the body. In some men the immune system mistakes these sperm as foreign proteins (antigens) and produces anti-sperm antibodies that are designed to target and interfere with sperm's motility (ability to move). Infections in the genital tract, such as inflammation of the testicles (orchitis) or sexually transmitted diseases, increase the risk for anti-sperm antibodies. The anti-sperm response itself appears to be a problem only if a man wishes to reverse the vasectomy.
Chronic Pain. Some men develop testicular pain following vasectomy. If this pain lasts longer than 3 months, it is referred to as post-vasectomy pain syndrome (PVPS). The causes of PVPS are unclear. It may be due to obstruction and resulting contraction of the epididymal duct, or inflammation and formation of fibrous tissue after rupture in the duct, which can cause nerve damage. Sperm granuloma has also been discussed as a possible cause, although their role remains controversial.
PNVS is first treated conservatively, with heat or cold therapy, rest, scrotal support, and nonsteroidal anti-inflammatory drugs (NSAIDs). Most patients are successfully treated with conservative therapies. If these methods do not work, other drug therapies (including injections of local anesthetics or steroids) may be tried. Transcutaneous electrical nerve stimulation (TENS) is another method that has been used with good results. If all options fail, surgical interventions [including removal of the epididymis (epididymectomy), granuloma excision, or vasectomy reversal surgery] may be required.
Cancer Concerns. At one time, there was concern that vasectomy might increase the risk of prostate cancer. Men with a family history of prostate cancer can discuss the risks and benefits of vasectomy with their doctors, but evidence indicates there is no link between vasectomy and prostate cancer. There was also some concern that vasectomy might increase the risk for testicular cancer. Studies have not identified any association between the two.
Reversal Surgery (Vasovasostomy and Vasoepididymostomy)
Although men should consider vasectomy a permanent decision, reversal procedures can restore fertility in some men who change their minds. The main reasons for requesting a vasectomy reversal are remarriage or the death of a child.
Vasectomy reversal can also sometimes provide pain relief for some of the small number of men who suffer post-vasectomy pain, but these patients should first be treated with pain management therapies. For men who desire a vasectomy reversal for psychological reasons, counseling is a better option.
Vasovasostomy Reversal Surgery Procedures
There are two types of vasectomy reversal surgical procedures:
- Vasovasostomy. The severed ends of the vas deferens are sewn back together.
- Vasoepididymostomy. The vas deferens is surgically reattached directly to the epididymis. This procedure is more difficult to perform and is used when vasovasostomy cannot be performed or does not work.
These procedures help restore sperm flow so that sperm can be ejaculated out of the urethra. Both types of procedures are performed on an outpatient basis, and the patient can return home the same day.
It is not possible to know in advance which procedure will be performed. The surgeon will make the decision whether to use vasovasostomy or vasoepididymostomy based on a fluid sample taken at the start of the operation. The fluid is removed from the vas end closest to the testicle and examined for its appearance and the presence of sperm.
If sperm are present or the fluid is clear, it indicates that there is no blockage in the epididymis, and a vasovasostomy can be performed. No sperm, or a creamy, thick appearance of fluid, is a sign of blockage, and the vasoepididymostomy surgical approach to bypass the blockage should be used. Other factors may also determine the surgeon's choice of reversal surgical procedure. In some cases, a combination of the two surgeries may be used, with vasovasostomy performed on one side and vasoepididymostomy on the other side.
Vasovasostomy. Vasovasostomy uses several different surgical approaches. Usually a microsurgical technique is used, in which a microscope helps magnify the surgical area. Vasovasostomy takes 2 - 3 hours to perform. The patient is given local anesthesia and a mild sedative.
Vasoepididymostomy. Vasoepididymostomy is a more complex microsurgical technique. To appreciate the difficulty of this operation, one should realize that the epididymis is 1/300th of an inch wide with a wall thickness of 1/1000th of an inch. Microscopic techniques are critical for the success of this procedure and require a surgeon who specializes in them. Vasoepididymostomy takes up to 4 hours to perform. The patient is given either general anesthesia or an epidural block.
Recovery and Follow-Up
Pain after reversal surgery is usually not severe and can be controlled with mild analgesics such as acetaminophen (Tylenol, generic). A cold pack placed on the scrotum area can help relieve swelling. Your doctor may recommend that you wear a jockstrap for a few weeks to help provide compression and to keep the surgical incisions in place. Most patients can return to work and resume normal non-strenuous activities within a week, but patients may need to refrain from heavy lifting and other rigorous physical activities for up to 4 weeks following surgery. Patients should wait 2 - 4 weeks before having sex.
The doctor will perform a semen analysis every 2 - 3 months after reversal surgery to check your sperm count. It generally takes about 2 months for sperm to reappear following vasovasostomy, and about 3 - 15 months following vasoepididymostomy. Either a stabilized sperm count, or pregnancy, indicates successful reversal surgery.
If reversal surgery is not successful, a repeat surgery can be performed. However, the success rates for repeat reversals are lower than for an initial reversal.
Pregnancy Results after Reversal Surgery
Vasectomy reversal restores sperm production in about 80 - 90% of men. On average, about 50% of couples achieve a pregnancy within 1 - 2 years after reversal surgery. Microsurgical techniques appear to help produce higher quality grade of sperm and better pregnancy rates than macrosurgical techniques. Several other factors determine the likelihood of a successful outcome. The experience of the surgeon is one critical factor. The time interval between the original vasectomy and the reversal procedure is another important factor. The shorter the time between vasectomy and reversal, the better the chances for fertility recovery.
Sperm removed during vasovasostomy can be frozen and used for assisted reproductive technologies in case of unsuccessful reversal surgery. If reversal surgery is not successful, a doctor may also be able to retrieve sperm from the testes or epididymis using various sperm retrieval techniques such as testicular fine needle aspiration, microsurgical epididymal sperm aspiration, percutaneous epididymal sperm aspiration, or testicular sperm extraction. [For more information, see In-Depth Report #67: Infertility in men.]
Intracytoplasmic Sperm Injection (ICSI)
The best assisted reproductive technology procedure for men who have had vasectomies or failed reversal surgery is intracytoplasmic sperm injection (ICSI). The procedure involves injecting a single sperm into an egg. The fertilized egg is then implanted in the woman using in vitro infertilization (IVF). [For more information, see In-Depth Reports #67 Infertility in men and #22 Infertility in women.]
Some men may consider pursuing ICSI in place of vasectomy reversal surgery. Even though the introduction of ICSI has helped improve pregnancy rates after vasectomy, reversal surgery is usually still a better choice for most men who want children. Reversal surgery costs less than ICSI and men have the potential to achieve long-lasting fertility. However, ICSI may be more effective than reversal surgeries in men whose vasectomies were performed at least 15 years earlier.
ICSI is performed a limited number of times, and the success rates are best if the women is younger than age 37. ICSI/IVF increases the chance for multiple births, which can pose risks to the mother and babies. Some research suggests that ICSI may increase the risk for birth defects more than IVF.
Resources
- www.plannedparenthood.org -- Planned Parenthood
- www.auanet.org -- American Urological Association
- www.urologyhealth.org -- Urology Health
- www.vasectomy.com -- Information on vasectomy
References
Adams CE, Wald M. Risks and complications of vasectomy. Urol Clin North Am. 2009 Aug;36(3):331-6.
Cook LA, Pun A, van Vliet H, Gallo MF, Lopez LM. Scalpel versus no-scalpel incision for vasectomy. Cochrane Database Syst Rev. 2007 Apr 18;(2):CD004112.
Cook LA, Van Vliet H, Lopez LM, Pun A, Gallo MF. Vasectomy occlusion techniques for male sterilization. Cochrane Database Syst Rev. 2007 Apr 18;(2):CD003991.
Davies MJ, Moore VM, Willson KJ, Van Essen P, Priest K, Scott H, Haan EA, Chan A. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012 May 10;366(19):1803-13. Epub 2012 May 5..
Nagler HM, Jung H. Factors predicting successful microsurgical vasectomy reversal. Urol Clin North Am. 2009 Aug;36(3):383-90.
Peterson HB. Sterilization. Obstet Gynecol. 2008 Jan;111(1):189-203.
Practice Committee of American Society for Reproductive Medicine. Vasectomy reversal. Fertil Steril. 2008 Nov;90(5 Suppl):S78-82.
Sharlip ID, Belker AM, Honig S, Labrecque M, Marmar JL, Ross LS, et al. Vasectomy: AUA Guideline. J Urol. 2012 Dec;188(6 Suppl):2482-91. Epub 2012 Oct 24.
Shih G, Turok DK, Parker WJ. Vasectomy: the other (better) form of sterilization. Contraception. 2011 Apr;83(4):310-5. Epub 2010 Oct 8.
Shridharani A, Sandlow JI. Vasectomy reversal versus IVF with sperm retrieval: which is better? Curr Opin Urol. 2010 Nov;20(6):503-9.
Sokal DC, Labrecque M. Effectiveness of vasectomy techniques. Urol Clin North Am. 2009 Aug;36(3):317-29.
Tandon S, Sabanegh E Jr. Chronic pain after vasectomy: a diagnostic and treatment dilemma. BJU Int. 2008 Jul;102(2):166-9. Epub 2008 Jul 1.
|
Review Date:
12/17/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |




